Quality of life and relationships in chronic prostatitis/chronic pelvic pain syndrome: models of self-regulation and psychosocial risk factors
Alison Crawford 2
J. Curtis Nickel 3
1 Psychology, Anesthesia & Urology, Queen's University, Kingston, Canada
2 Department of Psychology, Queen's University, Kingston, Canada
3 Department of Urology, Queen's University, Kingston, Canada
Abstract
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a condition marked by persistent pain in the perineum, pelvic area, and/or genitalia. The etiology of CP/CPPS remains unknown, making it a difficult to diagnose and to treat. CP/CPPS should not be viewed solely as a physical phenomenon, as psychological and social factors impact the patient’s experience of the disease. Instead, examining CP/CPPS from a biopsychosocial perspective lets us understand illness as a dynamic process that integrates biological, psychological, and social variables that can perpetuate the patient’s pain experience. This chapter is aimed at exploring biopsychosocial factors like catastrophizing, depression, and social relationships that affect quality of life in men living with CP/CPPS. These factors all come together under the umbrella of self-regulation theory and how patients with CP/CPPS cope with their symptoms and their pain. The self-regulation theory suggests that the way patients cope with their illness is influenced by how illness appraisals as well as the patients’ beliefs about how to cope effectively. Psychosocial interventions targeting patients’ ability to self-regulate and cope with their symptoms are explored as a way to improve their quality of life and to help manage painful experiences. Finally, this chapter identifies other biopsychosocial factors that warrant exploration in future research. Understanding how the mechanisms of the biopsychosocial perspective can affect the experience of CP/CPPS will not result in a cure. However, understanding the way in which biopsychosocial factors interact can help inform ways of improving patient quality of life, decreasing symptom related disability, and improving coping with chronic pain.
Introduction
Pain is a complex blend of physical sensation, emotions, and thoughts. It is these elements that impact medical diagnoses and treatment by consulting physicians. Whether it is an emergency room visit, an outpatient visit, and/or inpatient stay, these pain factors have all been tied to increased healthcare utilization [1], [2]. These blended features of experience have been summarized by the International Association for the Study of Pain defining pain as, “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” [3].
Pain is often described in terms of its sensory components (e.g., burning, throbbing), but the expression and impact of pain vary considerably by the cognitive and biological traits of the individual and their environment [4]. Cognitive-behavioral pain models are commonly used to guide interventions for chronic pain, where the role, and often the absence of, coping skills are emphasized. Patient self-regulation is a key process in any type of chronic pain management. Indeed, the patient’s self-awareness and problem solving ability mold their pain interpretations along with their management strategies [5], [6]. For example, when patients believe they are unable to self-manage a situation or physical sensation and their environment is not supportive, feelings of anxiety and appraisals of helplessness may arise to varying degrees, which can exacerbate pain. This chapter focuses on several empirically supported pain-associated psychosocial risk factors for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). This chapter presents models and research to help understand risk factor impact on quality of life, pain, and relationships in men suffering from CP/CPPS.
What is CP/CPPS?
Although common, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) has a well-deserved reputation among patients and physicians for being difficult to diagnose and categorize [7]. Prevalence estimates indicate that CP/CPPS is one of the most common urological conditions for men and that symptoms range considerably across socioeconomic status, race, and age [8]. Prostatitis accounts for 8% of urology outpatient visits in the United States and 3% in Canada [9]. The North American prevalence of CP/CPPS symptoms varies between 2–16% [5], [8]. Similar prevalence rates can be found internationally, with previous studies estimating rates of 5% in Japan, 8% in China, 14% in Italy, 8% in Australia, and 12% in Nigeria [10], [11], [12], [13], [14]. Although symptoms become most prominent at 35–65 years of age, they range widely [8], [15].
The National Institutes of Health define CP/CPPS as pelvic pain for 3 of the previous 6 months, with or without voiding symptoms, and with no evidence of uropathogenic bacterial infection [9]. The hallmark symptom of CP/CPPS is persistent pain in the perineum, pelvic area, and/or genitalia [5], [8]. CP/CPPS symptoms can vary, with most men reporting acute pain, longstanding persistent pain, or some combination of the two [9]. Comparable to other chronic pain conditions, the etiology of CP/CPPS and the related pain is unknown, making CP/CPPS a set of symptoms rather than specific disease [16], [17], [18].
Prostatitis can be either bacterial or abacterial. Acute and chronic bacterial prostatitis (i.e., category 1 & category 2 respectively) are the best known and least common of the prostatitis syndromes. CP/CPPS, with or without inflammation, is the third category of prostatitis syndrome with category 3A manifesting noted inflammation, but no evidence of infection. Category 3B, which has no noted inflammation, is regarded as the most common but least understood of the categories [19]. The fourth category is asymptomatic inflammatory prostatitis in which white blood cells are present in semen, expressed prostatic secretions (EPS) or post prostate massage urine samples (VB3) but with no associated pain.
CP/CPPS may not routinely remit, with 66% of community-based samples reporting symptoms one year later, and urology outpatients showing no reduction in pain, disability, or catastrophizing over a multi-year assessment [9], [20]. CP/CPPS cure successes are rather bleak, with monotherapy methods considered less than optimal [21]. The quality of life for men with CP/CPPS is diminished to levels comparable to patients with severe illnesses [22], [23]. Reviews of quality of life outcomes suggest that psychiatric disorders also strongly coexist with CP/CPPS [24]. Research supports a biopsychosocial model, as opposed to a biomedical focused model, for CP/CPPS pain and quality of life, with psychosocial risk factors such as pain catastrophizing given a prominent position [6], [25].
Biopsychosocial models
Persistent pain should not be viewed as solely a physical or a psychological phenomenon. The biomedical model for CP/CPPS has been criticized for its ineffectiveness in symptom management [21]. The data suggest that the experience and perception of pain is complex and maintained by biomedical, psychosocial, and behavioral variables whose associations are likely to evolve overtime within any one person. A biopsychosocial model outlines illness as a dynamic and reciprocal process, and integrates alternative physiological, psychological, and social–contextual variables that may affect and/or perpetuate pain. This model provides advantages over the biomedical model, especially when examining patient reactivity to pain, by considering multiple facets of the patient’s experience, including physical function, demographic information (e.g., age, race, socioeconomic status), cognitive/behavioral functioning, and the impact of the patient’s environment. The integration of psychosocial interventions can contribute to better patient outcomes. For example, an eight-week psychosocial management program for CP/CPPS, designed to teach patients to identify/dispute catastrophic thinking and to encourage health-focused behaviors, has demonstrated reductions in patient pain, disability, and catastrophizing [26]. The authors suggest that by targeting both physical and psychosocial contributions to the patient experience, overall patient outcomes can be improved. Below we will explore some of the psychosocial factors that are important in predicting patient outcome, including catastrophizing, depression, and social relations. We will then discuss self-regulation theory, coping and avenues for a biopsychosocial focused treatment for CP/CPPS that can be implemented.
Catastrophizing
Pain-related catastrophizing is a negative, exaggerated cognitive schema engaged in when a patient is in, or anticipates, pain [27]. Catastrophizing is assessed using the Pain Catastrophizing Scale, and captures three interrelated factors: rumination (inability to redirect thoughts away from the pain), magnification (expectancies for negative outcomes), and helplessness [27]. Rumination and magnification tend to be reactionary or proximal cognitive responses to pain, whereas helplessness may develop following persistent ruminative thoughts and or protracted pain. There is little doubt that helplessness about one’s pain and your perceived ability to manage it is associated with feelings of despair.
Catastrophizing is long known in the pain literature as a robust pain predictor in clinical and nonclinical samples [27]. The first CP/CPPS catastrophizing study showed that it was associated with greater disability, depression, urinary symptoms, and pain [6]. Further, the helplessness factor was the strongest pain predictor, even when urinary symptoms and depression were controlled. Indeed, variables related to quality of life, mood, catastrophizing and the presence of widespread somatic symptoms showed the largest effect sizes when patients with urologic chronic pelvic pain syndrome (UCPPS) were compared to healthy controls [28]. Diminished mental quality of life in men with CP/CPPS has also been predicted by greater helplessness and lower support from friends and family, even when demographics, medical status, and other psychosocial variables where controlled [25]. Helplessness is a predominant pain and quality of life predictor in CP/CPPS, commonly reported by patients with longer pain durations (four to seven years) [29]. The literature suggests that experiencing chronic symptoms, like pain, while also receiving no effective standard medical therapy may generate this helplessness in patients over time [30].
Evaluations of quality of life, pain, and psychosocial factors affecting CP/CPPS experience indicated stability in significant depression and anxiety, in that pain, disability, and catastrophizing did not improve over a two-year period [20]. Further, catastrophizing was comparable to patients with whiplash, interstitial cystitis/bladder pain syndrome, and CP/CPPS [6], [31], [32]. Thus, in the absence of a psychosocial/catastrophizing intervention or a reduction in pain, CP/CPPS patients are likely to exhibit alarmingly steady negative affect and catastrophic thinking about pain for extended periods. Catastrophizing and its helplessness is most likely a product of feeling unable to affect positive changes in pain.
It is important to note that catastrophizing is not the only variable that makes patients more or less vulnerable to pain. There is an interaction between resilience and catastrophizing whereby those who are more resilient to pain and who also catastrophize less had the slowest growth in pain ratings over five minutes of tourniquet ischemia [33]. Cognitive and affective positivity also accounted for more of the variance in this experimentally induced pain condition than behavioral perseverance, suggesting that thoughts, feelings and attitudes about pain are more relevant in the moment than long-term beneficial health behaviours [33].
Depression
Mental health and depression have been long-standing concerns in urological health for decades. Depression and CP/CPPS are significantly comorbid [34]. With this in mind, psychological factors related to the distress experienced by men with urological conditions are an important area of research. The literature suggests that 80% of patients with CP/CPPS report some form of depression and that 5% of these men report suicidal thinking [34]. Pain and urinary symptoms are exacerbated by depression which can contribute to a diminished quality of life [35]. Depression has been described as a psychosomatic factor in the experience of CP/CPPS symptoms and depression, urinary scores, and pain are predictors of worse physical quality of life [24], [25], [36].
In a Taiwanese study, compared to controls with no history of pelvic pain, patients with CP/CPPS were at an increased risk of developing a depressive disorder over a three-year period [37]. In another study, men with CP/CPPS not only experienced more perceived stress and anxiety than asymptomatic controls, but they also had a significantly higher waking cortisol response, suggesting dysfunctional hypothalamic-pituitary-adrenal axis function [38].
There is no doubt that the difficulties experienced by patients with chronic pelvic pain are pervasive. In a study comparing healthy controls to men and women with UCPPS, those with chronic pelvic pain experienced higher anxiety and depression, a decreased quality of life, more difficulties with sleep and sexual functioning, higher levels of general stress, more childhood and adult trauma, worse coping with pain and illness, self-reported deficits in memory and concentration, and more widespread pain symptoms [28]. Compared to men with UCPPS, women with UCPPS had more deficits in physical aspects of quality of life, more childhood adversity and more nonurologic symptoms, including pain, suggesting that men and women experience UCPPS differently.
There is also some evidence that pre-existing depression leads to worse outcomes in chronic pain, however it is unclear whether baseline chronic pain affects outcomes in depression, and what variables mediate the relationship between pain and depression, especially in the CP/CPPS population [39]. It is also unclear whether urinary specific symptoms play a role in depression. Some studies have found that exclusively pain, not urinary symptoms, are associated with depression, and that pain and urinary symptoms in UCPPS should be assessed and interpreted separately [40]. However, in other samples, pain and urinary symptoms predict depression when they are combined into one construct [41].
There needs to be future research to evaluate the relationship between pain, urinary symptoms, and depression, using more in depth item analyses. The role of certain personality traits (which are considered to be lifelong attributes), like negative emotionality, in mediating the development of chronic symptoms when faced with physical or environmental stress should also be explored [28]. There may also be a mechanism that underlies both physical vulnerability to chronic pain and/or inflammation and psychological vulnerability to depression, like early childhood adversity, or dysfunctional hypothalamic-pituitary-adrenal axis function [28], [38].
Social relations
By investigating spousal support for pain behaviour as buffering agents to poor patient outcomes such as pain or disability, research has provided some insights in how social support from spouses may be an important intervention target for patients with chronic pelvic pain. The supportive spousal coping behaviours are operationalized into couples’ interactions in the form of positive and negative responses to pain behaviour by significant others. Spousal responses can be classified by three categories: solicitous (e.g., tries to get me to rest), distracting (e.g., tries to get me involved in some activity) and negative (e.g., gets angry with me) [42]. When examined in men with CP/CPPS, solicitous responses from spouses (i.e., encouragement from their partners to rest when they were in pain) were associated with worse patient adjustment [43]. That is, at higher spouse solicitousness, patient pain was more highly associated with disability, indicating that greater solicitousness from a spouse should be avoided [43]. However, these results could also mean that spouses may be responding solicitously as a reaction to the patient’s pain and level of disability, where patients are physically incapable of completing certain tasks, and thus require the help of their spouse.
Some results also highlight sexuality as an issue in relationships of men with CP/CPPS. For example, reductions in frequency of sexual contacts have been reported in as much as 85% of men with CP/CPPS and more than 50% report periodic or total impotence in response to other symptoms like pain [44]. In comparison to the control males, men with CP/CPPS reported greater sexual dysfunction (i.e., less desire, more erectile problems, impaired orgasm, decreased sexual satisfaction) and greater symptoms of depression [45]. However, men with CP/CPPS in this sample did not report significantly decreased sexual satisfaction or relationship functioning when compared to male controls. These results suggest that men with CP/CPPS and their spouses may experience some sexual difficulties but that CP/CPPS may not have a large negative impact on patients’ intimate relationships.
The data reviewed here indicate that clinicians of men suffering from CP/CPPS should note the potential associations between patient sexual problems, relationship durations, and depressive symptoms. There is evidence for an intervention that can help the relationship satisfaction of couples in which one spouse suffers from chronic pain. Couples that were provided a motivational therapeutic assessment experienced significant decreases in pain, negative mood, and increases in martial satisfaction and positive mood from baseline to post-assessment compared to a control group who received education about the gate-control theory [46]. These findings could be applicable to couples with men suffering from CP/CPPS, and are an example of how psychosocial interventions play an important role in patient wellbeing.
Self-regulation theory and coping
The basic question we face now is, “how do these variables all come together?”, and the defining framework is one of self-regulation. A good self-regulator uses many different skills and dimensions of learning including their affect or moods, cognition and behavior. These areas interact with phases of forethought, performance and self-reflection tendencies depending on the interaction, which may affect observed behavior in a variety of manners [47], [48]. In its basic form, self-regulation theory describes an individual’s ability to control or cope with their thoughts, feelings and behaviors [49]. Self-regulation theory suggests that coping is influenced by appraisals of the stressor and beliefs about effective coping [50]. Lazarus and Folkman’s transactional stress model suggests that the chosen coping strategy is a result of a series of appraisals [51]. For example, as demonstrated in Figure 1, a chronic pain patient has perceived their pain as a stressor.
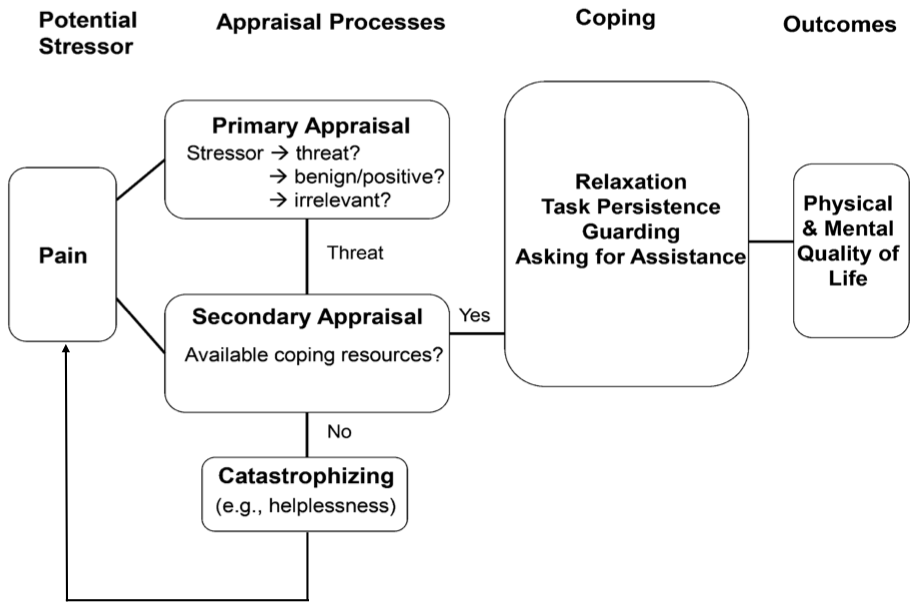
Figure 1: Self-regulation of pain
In their primary appraisal of the pain, they may interpret it as threatening, benign-positive, or irrelevant [52]. If the pain is considered a threat, then the individual engages in secondary appraisal. At this stage, the individual contemplates their available coping resources to manage the situation. Catastrophizing can also feedback into and exacerbate the patient’s pain experience. If the individual perceives that their coping resources are inadequate, negative appraisals can manifest such as feelings of helplessness.
We know that how a patient copes with their symptoms can contribute to a reduced quality of life. There are two main behavioral coping strategies now considered in the urologic research: “wellness-focused” or active coping and “illness-focused” or passive coping. Wellness-focused coping, such as relaxation and a person’s persistence to complete a chore or task, allows the individual to function despite pain [53]. Illness-focused coping, which involves behaviors such as adopting a sedentary lifestyle (i.e., pain-contingent resting) and guarding (i.e., taking comforting physical positions when in pain), may lead the individual to surrender control to symptoms like pain. Indeed, pain-contingent resting is a predictor of worse physical quality of life in patients with CP/CPPS [25]. Illness-focused coping has also been shown to be a mechanism that promotes higher pain and thus a reduced mental and physical quality of life in CP/CPPS [54]. Therefore, behavioral coping strategies play an important role in the management of CP/CPPS quality of life and depression.
Psychosocial intervention
Framing CP/CPPS in a self-regulation model allows for practical therapeutic implications for the management with the CP/CPPS patient, and based on the studies discussed above, discussions of patient catastrophizing and its meaning to the patient may be key. There are basic therapy models that can be applied to the practitioner-patient relationship in CP/CPPS [26]. Such modes of patient engagement can provide exceptionally valuable insights that can assist practitioners in managing patient fears and feelings of despair. For example, the practitioner can lead a conversation concerning pain catastrophizing by reviewing the subscales and the items of the Pain Catastrophizing Scale with patients. Using a similar therapy method as above, patient baseline scores showed significant linear reductions across 8-weeks for pain, disability, and catastrophizing [26]. CP/CPPS symptoms and quality of life were also significantly improved. Furthermore, the change in symptoms and psychosocial risk factors from baseline to 8-week termination were predicted by associated reductions in catastrophizing. These findings, however, were not statistically significant. This can be explained by the small sample size employed by the study. Referent to these findings, management for CP/CPPS risk factors is feasible and practitioner engagement is important.
Catastrophizing can be reduced. The practical implications for the findings above can also focus on conversations of the patient’s social interactions. As was suggested for the patient experiencing catastrophizing, opportunities to consider, reflect and problem solve potential issues regarding spousal support is recommended. As with the catastrophizing items, these can be reviewed or discussed by the patient and practitioner to initiate or lead a discussion into the types of support experienced and benefit of spousal support. The data is clear, men suffering from CP/CPPS or male mental health in general, are an underserviced group in need of psychological supports.
Cognitive behavioral therapy (CBT) is a form of psychological treatment that focuses on the relationship between thoughts, feelings and actions [26]. CBT has been found to reduce pain intensity, pain-related interference, disability, depression, and increase health-related quality of life in patients with chronic pain [55], [56]. One CBT self-management group designed for complex chronic conditions found that these groups can significantly reduce symptoms of pain, disability, depression and anxiety [57]. In these pain management groups, the primary goal for patients was to learn how to better cope with the ongoing pain that they experience, by shifting from passive to active coping. Women reported more active coping than men both before and after the pain management group, but the positive outcomes likely occur equally or both men and women [57]. This program is also equally helpful for patients with complex conditions and multiple diagnoses, making it a prime candidate for UCPPS conditions like CP/CPPS.
There have been many online programs based off of CBT techniques that have proven to be effective in reducing pain, disability, anxiety, depression, catastrophizing, stress, and increasing patient knowledge about chronic pain [58], [59]. Indeed, web-based CBT options are a viable option to explore, as they are less costly than in person therapies and do not appear to have many adverse side effects [60]. Although the benefits of the CBT have small to moderate effect sizes, further investigation into these types of treatments is warranted. CBT can be an individualized process, and it remains unclear which parts of the treatment are beneficial and for whom [61].
Areas for future research
As mentioned, CP/CPPS typically effects men between the ages of 35 and 65 years. However, research on North American male adolescents are alarming, suggesting as many as 8.3% report CP/CPPS [62]. Catastrophic magnification, or the internal cognitive exaggeration of the threat value of pain sensations, was unique amongst the catastrophizing domains in the prediction of worse adolescent quality of life. What is interesting in these adolescent findings is how they appear to compliment the report that catastrophic helplessness (i.e., thoughts that you can do little to manage your pain) and low social support predicted worse quality of life over and above pain and urinary symptoms in older men with long standing CP/CPPS [63]. The differential quality of life findings for catastrophizing in this adolescent sample (i.e., magnification) [62] versus the older sample report by Nickel et al. [25] (i.e., helplessness), may indicate a negative psychological progression in CP/CPPS. Magnification is a primary pain appraisal, often reported with short pain durations, while helplessness is a secondary appraisal tending to be present in self-reports with longer pain durations. This age and catastrophizing effect does present potential implications on differential treatment. Indeed, for this particular group of adolescents, a cognitive-behavioral treatment program seems to be indicated that would target catastrophizing about pain with a focus on thinking that magnifies pain while an older group may benefit more from the targeting of helplessness cognition. More research should be conducted on potential intervention strategies for adolescents with CP/CPPS, as their cognitive needs differ from the older population.
Another area of that merits further investigation is the role of abuse on CP/CPPS diagnosis. Results have indicated that men who reported previous abuse (i.e., sexual, physical, or emotional) had significantly greater odds of reporting CP/CPPS symptoms [64]. Interestingly, reports on the frequency of previous physical and emotional abuse were associated with increases in both pain and urinary domain scores on the NIH-CPSI. These startling data suggest for the first time that CP/CPPS symptoms, which are common in community samples of men, may be associated with previous abuse. Again, this is an interesting avenue for biopsychosocial treatment, as the needs of men with CP/CPPS who experienced abuse may be different from those who do not have that history.
Resilience is another area for future CP/CPPS research. In particular, it would be useful to examine how cognitive/affective positivity and behavioral perseverance predict pain while individuals with chronic pain are engaging in physical activity [33]. It would be most interesting to parse out the mechanisms of pain-specific resilience. Is resilience a trait that predisposes individuals to react in a way to better endure pain, or does resilience develop through learning how to cope adaptively to their pain? These answers are potentally important additions to the current research.
Future studies regarding psychological interventions for CP/CPPS might focus on positive psychology, and the enhancement of psychological states [65]. These types of interventions aim to promote overall health and well-being instead of focusing on problem-focused coping. Although there is limited evidence on the efficacy of this type of intervention, but it may be useful to patients with CP/CPPS, as it focuses on targeting mechanisms that improve emotional states and social relations through forgiveness, gratitude, kindness and compassion.
Finally, future research for both medical and psychological interventions could focus on social factors, as pain always occurs in their context, but this context is often ignored [65]. Another part of the literature to keep in mind is that patients who are positive on the RICE diagnostic criteria for UCPPS are more likely to experience nonurological associated somatic syndrome and more severe symptoms [66]. This is a potential confounding factor that must be kept in mind for future CP/CPPS research, even though nonurological associated somatic syndromes are more common in women.
Conclusion
The symptoms associated with CP/CPPS can have a profound effect on patient quality of life. This may begin in adolescence and manifest greater impact later in adulthood as a chronic treatment refractory pain condition that is difficult to manage and remains to be seen in longitudinal studies of men. Both the symptoms of CP/CPPS (e.g., pain) and patient quality of life are significantly influenced by cognitive “thinking traps” such as catastrophizing, or mood states such as depression and anxiety. By considering CP/CPPS in the context of a biopsychosocial model, clinicians can expand the therapeutic options for their patients through psychosocial interventions directed self-regulatory processes towards stress and negative mood reduction. Our increasing understanding of the biopsychosocial model may not result in cure, but should realize our goal of improving patient quality of life, decreasing symptom based disability, and coping with chronic pain in men suffering from CP/CPPS.
References
[1] Turk DC, Dworkin RH. What should be the core outcomes in chronic pain clinical trials? Arthritis Res Ther. 2004;6(4):151-4. DOI: 10.1186/ar1196[2] Hasselström J, Liu-Palmgren J, Rasjö-Wrååk G. Prevalence of pain in general practice. Eur J Pain. 2002;6(5):375-85. DOI: 10.1016/S1090-3801(02)00025-3
[3] Bonica JJ. The need of a taxonomy. Pain. 1979 Jun;6(3):247-8. DOI: 10.1016/0304-3959(79)90046-0
[4] Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001 Mar;17(1):52-64. DOI: 10.1097/00002508-200103000-00008
[5] Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999 Jul;282(3):236-7.
[6] Tripp DA, Nickel JC, Wang Y, Litwin MS, McNaughton-Collins M, Landis JR, Alexander RB, Schaeffer AJ, O’Leary MP, Pontari MA, Fowler JE Jr, Nyberg LM, Kusek JW; National Institutes of Health-Chronic Prostatitis Collaborative Research Network (NIH-CPCRN) Study Group. Catastrophizing and pain-contingent rest predict patient adjustment in men with chronic prostatitis/chronic pelvic pain syndrome. J Pain. 2006 Oct;7(10):697-708. DOI: 10.1016/j.jpain.2006.03.006
[7] Nickel JC. The Prostatitis Manual: a Practical Guide to Management of Prostatitis/Chronic Pelvic Pain Syndrome. Oxfordshire: Bladon Medical Publishing; 2002.
[8] Schaeffer AJ, Datta NS, Fowler JE Jr, Krieger JN, Litwin MS, Nadler RB, Nickel JC, Pontari MA, Shoskes DA, Zeitlin SI, Hart C; Chronic Prostatitis Collaborative Research Network. Overview summary statement. Diagnosis and management of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Urology. 2002 Dec;60(6 Suppl):1-4. DOI: 10.1016/S0090-4295(02)01979-9
[9] Nickel JC, Downey JA, Nickel KR, Clark JM. Prostatitis-like symptoms: one year later. BJU Int. 2002 Nov;90(7):678-81. DOI: 10.1046/j.1464-410X.2002.03007.x
[10] Kunishima Y, Mori M, Kitamura H, Satoh H, Tsukamoto T. Prevalence of prostatitis-like symptoms in Japanese men: Population-based study in a town in Hokkaido. Int J Urol. 2006 Oct;13(10):1286-9. DOI: 10.1111/j.1442-2042.2004.01556.x
[11] Liang CZ, Li HJ, Wang ZP, Xing JP, Hu WL, Zhang TF, Ge WW, Hao ZY, Zhang XS, Zhou J, Li Y, Zhou ZX, Tang ZG, Tai S. The prevalence of prostatitis-like symptoms in China. J Urol. 2009 Aug;182(2):558-63. DOI: 10.1016/j.juro.2009.04.011
[12] Bartoletti R, Cai T, Mondaini N, Dinelli N, Pinzi N, Pavone C, Gontero P, Gavazzi A, Giubilei G, Prezioso D, Mazzoli S, Boddi V, Naber KG; Italian Prostatitis Study Group. Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multicenter case-control observational study. J Urol. 2007 Dec;178(6):2411-5; discussion 2415. DOI: 10.1016/j.juro.2007.08.046
[13] Ferris JA, Pitts MK, Richters J, Simpson JM, Shelley JM, Smith AM. National prevalence of urogenital pain and prostatitis-like symptoms in Australian men using the National Institutes of Health Chronic Prostatitis Symptoms Index. BJU Int. 2010 Feb;105(3):373-9. DOI: 10.1111/j.1464-410X.2009.08708.x
[14] Ejike CE, Ezeanyika LU. Prevalence of chronic prostatitis symptoms in a randomly surveyed adult population of urban-community-dwelling Nigerian males. Int J Urol. 2008 Apr;15(4):340-3. DOI: 10.1111/j.1442-2042.2008.02003.x
[15] Collins MM, Stafford RS, O'Leary MP, Barry MJ. Distinguishing chronic prostatitis and benign prostatic hyperplasia symptoms: results of a national survey of physician visits. Urology. 1999 May;53(5):921-5. DOI: 10.1016/S0090-4295(98)00636-0
[16] Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb;344(5):363-70. DOI: 10.1056/NEJM200102013440508
[17] Nickel JC. Chronic prostatitis/chronic pelvic pain: the syndrome. J Urol. 2009 Jul;182(1):18-9. DOI: 10.1016/j.juro.2009.04.052
[18] Nickel JC. Words of wisdom. Re: Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Eur Urol. 2009 Nov;56(5):881. DOI: 10.1016/j.eururo.2009.08.005
[19] Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001 Mar;165(3):842-5. DOI: 10.1016/S0022-5347(05)66541-X
[20] Tripp DA, Nickel JC, Shoskes D, Koljuskov A. A 2-year follow-up of quality of life, pain, and psychosocial factors in patients with chronic prostatitis/chronic pelvic pain syndrome and their spouses. World J Urol. 2013 Aug;31(4):733-9. DOI: 10.1007/s00345-013-1067-6
[21] Nickel JC, Downey J, Ardern D, Clark J, Nickel K. Failure of a monotherapy strategy for difficult chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004 Aug;172(2):551-4. DOI: 10.1097/01.ju.0000131592.98562.16
[22] McNaughton Collins M, Pontari MA, O'Leary MP, Calhoun EA, Santanna J, Landis JR, Kusek JW, Litwin MS; Chronic Prostatitis Collaborative Research Network. Quality of life is impaired in men with chronic prostatitis: the Chronic Prostatitis Collaborative Research Network. J Gen Intern Med. 2001 Oct;16(10):656-62. DOI: 10.1111/j.1525-1497.2001.01223.x
[23] Wenninger K, Heiman JR, Rothman I, Berghuis JP, Berger RE. Sickness impact of chronic nonbacterial prostatitis and its correlates. J Urol. 1996 Mar;155(3):965-8. DOI: 10.1016/S0022-5347(01)66359-6
[24] Ku JH, Kim SW, Paick JS. Quality of life and psychological factors in chronic prostatitis/chronic pelvic pain syndrome. Urology. 2005 Oct;66(4):693-701. DOI: 10.1016/j.urology.2005.04.050
[25] Nickel JC, Tripp DA, Chuai S, Litwin MS, McNaughton-Collins M, Landis JR, Alexander RB, Schaeffer AJ, O'Leary MP, Pontari MA, White P, Mullins C, Nyberg L, Kusek J; NIH-CPCRN Study Group. Psychosocial variables affect the quality of life of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2008 Jan;101(1):59-64. DOI: 10.1111/j.1464-410X.2007.07196.x
[26] Tripp DA, Nickel JC, Katz L. A feasibility trial of a cognitive-behavioural symptom management program for chronic pelvic pain for men with refractory chronic prostatitis/chronic pelvic pain syndrome. Can Urol Assoc J. 2011 Oct;5(5):328-32. DOI: 10.5489/cuaj.10201
[27] Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 1995;7(4): 524-532. DOI: 10.1037/1040-3590.7.4.524
[28] Naliboff BD, Stephens AJ, Afari N, Lai H, Krieger JN, Hong B, Lutgendorf S, Strachan E, Williams D; MAPP Research Network. Widespread Psychosocial Difficulties in Men and Women With Urologic Chronic Pelvic Pain Syndromes: Case-control Findings From the Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network. Urology. 2015 Jun;85(6):1319-27. DOI: 10.1016/j.urology.2015.02.047
[29] Sullivan MJ, Stanish W, Sullivan ME, Tripp D. Differential predictors of pain and disability in patients with whiplash injuries. Pain Res Manag. 2002;7(2):68-74. DOI: 10.1155/2002/176378
[30] Tripp DA, Nickel JC. The psychology of urological chronic pelvic pain: A primer for urologists who want to know how to better manage chronic prostatitis and interstitial cystitis: Lesson 40, Volume 30. AUA Update Series. Linthicum, MD: American Urological Association; 2011.
[31] Sullivan MJ, Thibault P, Simmonds MJ, Milioto M, Cantin AP, Velly AM. Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for whiplash injuries. Pain. 2009 Oct;145(3):325-31. DOI: 10.1016/j.pain.2009.06.031
[32] Nickel JC, Tripp DA, Pontari M, Moldwin R, Mayer R, Carr LK, Doggweiler R, Yang CC, Mishra N, Nordling J. Interstitial cystitis/painful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. J Urol. 2010 Oct;184(4):1358-63. DOI: 10.1016/j.juro.2010.06.005
[33] Slepian PM, Ankawi B, Himawan LK, France CR. Development and Initial Validation of the Pain Resilience Scale. J Pain. 2016 Apr;17(4):462-72. DOI: 10.1016/j.jpain.2015.12.010
[34] Alexander RB, Trissel D. Chronic prostatitis: results of an Internet survey. Urology. 1996 Oct;48(4):568-74. DOI: 10.1016/S0090-4295(96)00234-8
[35] Ku JH, Jeon YS, Kim ME, Lee NK, Park YH. Psychological problems in young men with chronic prostatitis-like symptoms. Scand J Urol Nephrol. 2002;36(4):296-301. DOI: 10.1080/003655902320248272
[36] Tripp DA, Curtis Nickel J, Landis JR, Wang YL, Knauss JS; CPCRN Study Group. Predictors of quality of life and pain in chronic prostatitis/chronic pelvic pain syndrome: findings from the National Institutes of Health Chronic Prostatitis Cohort Study. BJU Int. 2004 Dec;94(9):1279-82. DOI: 10.1111/j.1464-410X.2004.05157.x
[37] Chung SD, Huang CC, Lin HC. Chronic prostatitis and depressive disorder: a three year population-based study. J Affect Disord. 2011 Nov;134(1-3):404-9. DOI: 10.1016/j.jad.2011.05.046
[38] Anderson RU, Orenberg EK, Chan CA, Morey A, Flores V. Psychometric profiles and hypothalamic-pituitary-adrenal axis function in men with chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2008 Mar;179(3):956-60. DOI: 10.1016/j.juro.2007.10.084
[39] Williams A, Schäfer G. How do we understand depression in people with persistent pain? J Contemp Psychother. 2016;46(3):149-157. DOI: 10.1007/s10879-016-9325-8
[40] Griffith JW, Stephens-Shields AJ, Hou X, Naliboff BD, Pontari M, Edwards TC, Williams DA, Clemens JQ, Afari N, Tu F, Lloyd RB, Patrick DL, Mullins C, Kusek JW, Sutcliffe S, Hong BA, Lai HH, Krieger JN, Bradley CS, Kim J, Landis JR. Pain and Urinary Symptoms Should Not be Combined into a Single Score: Psychometric Findings from the MAPP Research Network. J Urol. 2016 Apr;195(4 Pt 1):949-54. DOI: 10.1016/j.juro.2015.11.012
[41] Katz L, Tripp DA, Nickel JC, Mayer R, Reimann M, van Ophoven A. Disability in women suffering from interstitial cystitis/bladder pain syndrome. BJU Int. 2013 Jan;111(1):114-21. DOI: 10.1111/j.1464-410X.2012.11238.x
[42] Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain. 1985 Dec;23(4):345-56.
[43] Ginting JV, Tripp DA, Nickel JC. Self-reported spousal support modifies the negative impact of pain on disability in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2011 Nov;78(5):1136-41. DOI: 10.1016/j.urology.2011.03.073
[44] Mehik A, Hellström P, Sarpola A, Lukkarinen O, Järvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001 Jul;88(1):35-8.
[45] Smith KB, Pukall CF, Tripp DA, Nickel JC. Sexual and relationship functioning in men with chronic prostatitis/chronic pelvic pain syndrome and their partners. Arch Sex Behav. 2007 Apr;36(2):301-11. DOI: 10.1007/s10508-006-9086-7
[46] Miller LR, Cano A, Wurm LH. A motivational therapeutic assessment improves pain, mood, and relationship satisfaction in couples with chronic pain. J Pain. 2013 May;14(5):525-37. DOI: 10.1016/j.jpain.2013.01.006
[47] Duckworth AL, Quinn PD, Seligman MEP. Positive predictors of teacher effectiveness. J Posit Psychol. 2009;4(6): 540-7. DOI: 10.1080/17439760903157232
[48] Schunk DH. Self-regulated learning: the educational legacy of Paul R. Pintrich. Educational Psychologist. 2005.40(2):85-94. DOI: 10.1207/s15326985ep4002_3
[49] Carver CS, Scheier M. On the self-regulation of behaviour. New York: Cambridge University Press; 1998. p. 439.
[50] Johnson JE. Self-regulation theory and coping with physical illness. Res Nurs Health. 1999 Dec;22(6):435-48.
[51] Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984.
[52] Sullivan MJ, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. 2001 Mar;91(1-2):147-54.
[53] Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987 Oct;31(1):53-64.
[54] Krsmanovic A, Tripp DA, Nickel JC, Shoskes DA, Pontari M, Litwin MS, McNaughton-Collins MF. Psychosocial mechanisms of the pain and quality of life relationship for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Can Urol Assoc J. 2014 Nov;8(11-12):403-8. DOI: 10.5489/cuaj.2179
[55] Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007 Jan;26(1):1-9. DOI: 10.1037/0278-6133.26.1.1
[56] Nicholas MK, Asghari A, Blyth FM, Wood BM, Murray R, McCabe R, Brnabic A, Beeston L, Corbett M, Sherrington C, Overton S. Self-management intervention for chronic pain in older adults: a randomised controlled trial. Pain. 2013 Jun;154(6):824-35. DOI: 10.1016/j.pain.2013.02.009
[57] Boschen KA, Robinson E, Campbell KA, Muir S, Oey E, Janes K, Fashler SR, Katz J. Results from 10 Years of a CBT Pain Self-Management Outpatient Program for Complex Chronic Conditions. Pain Res Manag. 2016;2016:4678083. DOI: 10.1155/2016/4678083
[58] Dear BF, Titov N, Perry KN, Johnston L, Wootton BM, Terides MD, Rapee RM, Hudson JL. The Pain Course: a randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain. 2013 Jun;154(6):942-50. DOI: 10.1016/j.pain.2013.03.005
[59] Ruehlman LS, Karoly P, Enders C. A randomized controlled evaluation of an online chronic pain self management program. Pain. 2012 Feb;153(2):319-30. DOI: 10.1016/j.pain.2011.10.025
[60] Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917-29. DOI: 10.1016/j.jpain.2010.06.005
[61] Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012 Nov 14;11:CD007407. DOI: 10.1002/14651858.CD007407.pub3
[62] Tripp DA, Nickel JC, Ross S, Mullins C, Stechyson N. Prevalence, symptom impact and predictors of chronic prostatitis-like symptoms in Canadian males aged 16-19 years. BJU Int. 2009 Apr;103(8):1080-4. DOI: 10.1111/j.1464-410X.2008.08157.x
[63] Nickel JC, Tripp D, Teal V, Propert KJ, Burks D, Foster HE, Hanno P, Mayer R, Payne CK, Peters KM, Kusek JW, Nyberg LM; Interstitial Cystitis Collaborative Trials Group. Sexual function is a determinant of poor quality of life for women with treatment refractory interstitial cystitis. J Urol. 2007 May;177(5):1832-6. DOI: 10.1016/j.juro.2007.01.060
[64] Hu JC, Link CL, McNaughton-Collins M, Barry MJ, McKinlay JB. The association of abuse and symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome: results from the Boston Area Community Health survey. J Gen Intern Med. 2007 Nov;22(11):1532-7. DOI: 10.1007/s11606-007-0341-y
[65] Sturgeon JA, Zautra AJ. Social pain and physical pain: shared paths to resilience. Pain Manag. 2016;6(1):63-74. DOI: 10.2217/pmt.15.56
[66] Krieger JN, Stephens AJ, Landis JR, Clemens JQ, Kreder K, Lai HH, Afari N, Rodríguez L, Schaeffer A, Mackey S, Andriole GL, Williams DA; MAPP Research Network. Relationship between chronic nonurological associated somatic syndromes and symptom severity in urological chronic pelvic pain syndromes: baseline evaluation of the MAPP study. J Urol. 2015 Apr;193(4):1254-62. DOI: 10.1016/j.juro.2014.10.086




