Author's preferred treatment
1 Hand Surgery, University Hospital Southampton, Southampton, United Kingdom
This section has described the various options for treating Dupuytren’s Disease. Every case is different. Moreover every surgeon has a different training, a different talent and a different philosophy. So it is not possible to provide a cook book recipe for all cases of DD – the treatment must be individualised.
Certain points should be considered:
Risk
The treatment of DD necessarily carries a risk of complications (Table 1).
| Complication | Needle fasciotomy |
Collagenase | Fasciectomy | Skin graft |
|---|---|---|---|---|
| Nerve damage | + | - | +++ | +++ |
| Infection | - | - | + | + |
| Stiffness | - | - | ++ | ++ |
| Wound failure/split | ++ | +++ | + | + |
| Blood blister | + | ++ | - | - |
| Recovery time | + | + | +++ | ++ |
| Tendon rupture | + | + | - | - |
| Recurrence | ++++ | +++ | +++ | + |
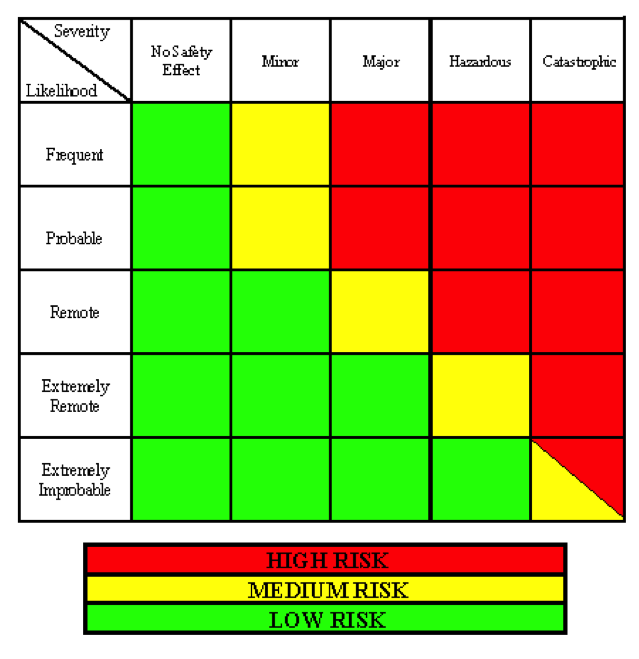
When calculating risk, one must balance the frequency of that risk with the severity of that risk (Table 2).
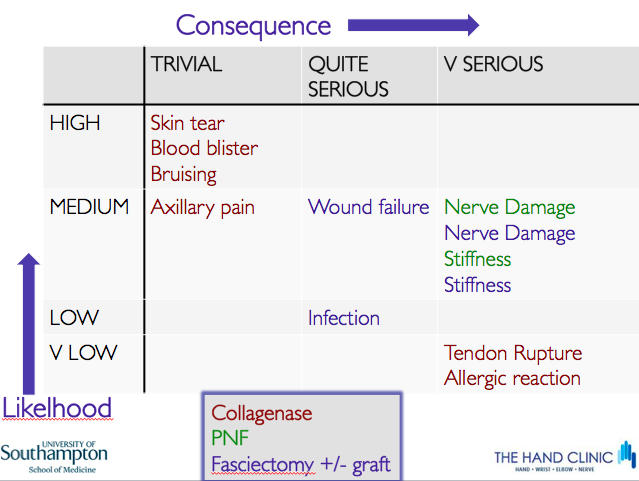
Thus with the treatment of DD, a risk such as an allergic reaction to CCH is very rare but potentially catastrophic; a skin tear with PNF is very common but of no clinical consequence (Table 3). So patients must be carefully advised about the potential risks of their treatment and they must provide their written consent
Recurrence
DD has a modest (fasciectomy), high (CCH) or very high (PNF) tendency to recur; However, a full thickness skin graft has the lowest chance of recurrence. Only if the cords remain suitable (i.e. discrete), re-treatment after PNF or CCH with PNF or CCH is usually satisfactory combining the innate advantages of simplicity, prompt recovery and low complications. Surgery after CCH is usual no more challenging than primary surgery.
Whilst fasciectomy (probably) has a lower recurrence rate than PNF or CCH, if recurrence does occur then a more difficult operation is needed – surgery must deal with not only the recurrent disease but also the scarring from the previous procedures.
Cost
The modern surgeon is obliged to take responsibility for the costs of healthcare. In financially strained times, if we spend too much money on one treatment then there will be not enough money for someone else’s treatment. Before even offering treatment for DD, one must really consider whether treatment is justified at all. For many patients DD is nothing more than a cosmetic blemish of no consequence. Just because we have a treatment does not necessarily mean that the healthcare system has to fund it and deprive the funds that could be used for a condition of much greater clinical relevance.
So the cost can, in my opinion, only be justified if the patient has, or soon will have, significant difficulties and if the risks of treatment are fully accepted (because complications will add to the cost and also expose the system to medicolegal costs as well …)
The cost analysis is very complex- the quick recovery from CCH with regards to working and paying tax again may justify the apparent expense of the drug; the slightly greater cost of skin grafting (slightly longer surgery, slightly more post-operative attention to therapy and dressings) may be justified by not having to pay the cost of a second fasciectomy.
My preferred approach
So in my opinion, treatment should not be offered for cosmetic reasons and trivial functional problems.
For diffuse uncomfortable palmar disease, I refer for radiotherapy. For palmar nodules, excision under local anaesthetic is preferred. For discrete cords in older, lower demand patients, PNF is cheap and rewarding. For discrete cords across one or two joints and especially natatory cords, CCH is currently proving to be reliable and effective. I find that properly consented patients whose cords are equally suitable for PNF, CCH or fasciectomy, almost never prefer surgery.
In those with multiple digits and more diffuse disease, and especially those with a diathesis, I usually advise fasciectomy with full thickness grafting. This is because dermofasciectomy with skin graft is not really much more difficult technically than fasciectomy, nor is the post-operative recovery particular more onerous. By making the small effort to do this slightly bigger procedure first, the surgeon will minimise the chance of that more difficult second operation which would be needed for the proportion who inevitably recur after simple fasciectomy.



