[Handover quality in paper-based and electronic nursing documentation: A quantitative study in a pre-post-design]
Sophia Schießer 1Daniel Flemming 2
Bernd Reuschenbach 2
1 Helios Amper-Klinikum Dachau, Dachau, Germany
2 Katholische Stiftungshochschule München, Munich, Germany
Abstract
To meet the numerous challenges of 21st-century healthcare, an increasing number of hospitals are adopting digital documentation systems. As a result, electronic nursing documentation is becoming increasingly important in the transfer of patient information. This study quantitatively analyzed the quality of handovers before and after the implementation of electronic nursing documentation at Helios Klinikum Munich West. The analysis showed that, although a slight improvement in handover quality was observed after implementation, no statistically significant enhancement could be confirmed. Possible explanations for this may include methodological limitations and inherent challenges of digitalization.
Keywords
patient handover, documentation, nursing informatics, digital technology, data analysis, Germany
Introduction
Faced with the growing challenges of 21st-century healthcare, an increasing number of hospitals are turning to digital documentation systems [1], [2]. Shift handovers, being both complex and prone to errors, serve as a critical interface for information exchange between healthcare providers [3], [4]. While numerous studies have explored the impact of electronic health records on various nursing processes, there is limited evidence on how the introduction of electronic nursing documentation affects handover quality [5]. This study addresses this research gap by examining the impact of implementing a digital documentation system on handover quality at Helios Klinikum München West.
Background and objectives
The importance of electronic nursing documentation and handover processes
In October 2020, the German Hospital Future Fund (Krankenhauszukunftsgesetz) was enacted. Since early 2021, Germany has invested € 4.3 billion in nationwide hospital digitalization projects, focusing on four key areas: “digital infrastructure”, “telemedicine, sensor technology, and robotics“, “digitalization of medical service units“, and “networking and interoperability“ [6]. This funding aims to accelerate the digital transformation of German hospitals. The long-term objective is to enhance digitalization to ensure high-quality, safe, comprehensive, cross-sectoral, and efficient healthcare [6].
The specific funding measures include, among others, the establishment of a continuous, structured electronic documentation system for nursing and treatment services, as well as the implementation of automated and speech-based documentation systems to support these services [6]. Since nursing represents the largest professional group in hospitals and a central component of all hospital processes, increasing the availability of nursing and treatment documentation aims to relieve nursing staff in care planning, care documentation, and decision support. Additionally, communication and coordination processes among the various stakeholders involved in patient care should be simplified and made more secure [6], [7], [8], [9], [10]. An important contribution to ensuring safe patient care in terms of continuity of care is made by the handover as the transfer of nursing information between shifts [11]. The study by O’Connell et al. [3] points to heterogeneous assessments by nurses regarding the effectiveness of the handover process: Some nurses reported receiving sufficient patient information. Other nurses indicated that the subjectivity and inaccuracy of the information, the repetition of information, the duration of the handover, and the mention of irrelevant information need improvement [3].
In transforming the handover process through the implementation of digital solutions, the impacts on the process and the quality of the handover should always be evaluated, and a comprehensive information management concept should be considered [12].
Objective
Based on this context, the aim of this study was to evaluate whether the handover quality between nursing shifts has improved following the implementation of electronic nursing documentation at Helios Klinikum München West.
Implementation of electronic nursing documentation
The implementation of electronic nursing documentation at Helios Klinikum München West occurred from October 19, 2021, to November 30, 2021. This implementation included the integration of applications for electronic nursing process documentation in acute inpatient care for adults (epaAC®) and for recording nursing services (LEP®) into the hospital information system i.s.h.med. Mobile ward rounds carts were introduced for mobile data entry and processing. The intervention did not include the complete digitalization of all paper-based documents in the inpatient setting. Prior to the introduction of electronic nursing documentation (as of July 2021), handovers typically took place orally between nurses using individually handwritten handover notes. Usually, nurses met at a central location on the ward at the end of a shift to exchange information about the current condition of patients. With the implementation of electronic nursing documentation (as of February 2022), the handover process changed in that handovers are still conducted verbally, but are now supported by direct access to the digital nursing documentation epaAC® and LEP®. During handovers, relevant digitally recorded patient information can be accessed in a structured and clear manner via the hospital information system i.s.h.med.
Methods
Design
In a pre-post design, quantitative data were collected to evaluate the handover quality before and after the implementation of electronic nursing documentation at Helios Klinikum München West. A written paper-based survey was conducted both prior to and after implementation, in July 2021 (t0) and approximately three months after implementation in February 2022 (t1), at Helios Klinikum München West.
Data collection
For data collection, the unpublished German translation of the Handover Evaluation Scale was used [13]. The translation followed the WHO guidelines “Process of Translation and Adaptation of Instruments”, including forward translation, back translation by native speakers, and a consensus conference for semantic adaptation in collaboration with the original author, O’Connell [13]. This approach can also be found in the ISPOR “Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures” [14]. The content and format of the Handover Evaluation Scale remained unchanged throughout this process (see Table 1 [Tab. 1]) [13]. Since patient handovers in the hospital typically do not take place at the bedside, the optional fourth subscale, which focuses on patient involvement, was omitted in accordance with O’Connell et al. [15]. The quality of handovers was assessed using a seven-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). In the survey at time point t1, an additional question was included: “In your opinion, has handover quality changed with electronic documentation compared to paper-based documentation?“ with response options “Yes”, “No“ and “Don’t know". Additionally, the question “If so, how has the quality of handovers with electronic documentation changed in your view?“ was included. The response options ranged on a five-point Likert scale from “Much worse” to “Much better”.
Table 1: Translation of Handover Evaluation Scale, adapted from [13] and [15]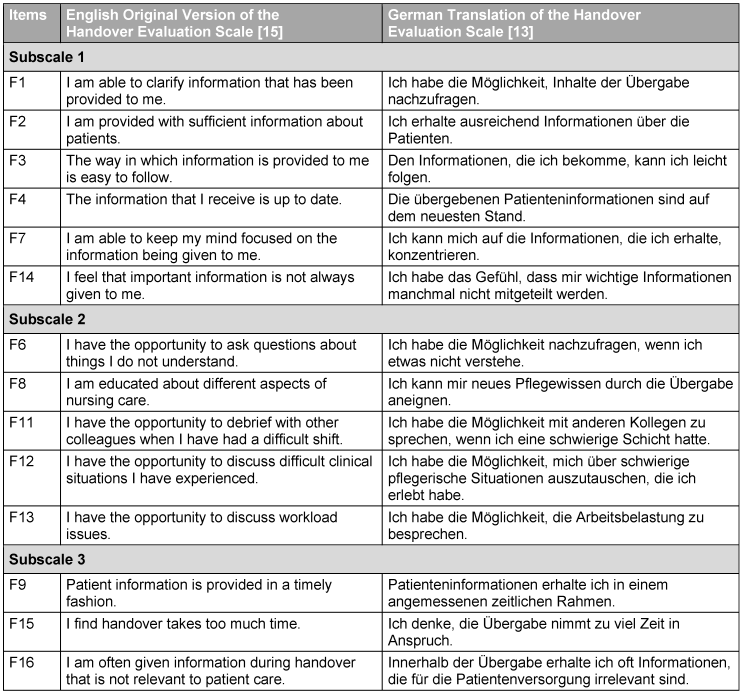
Furthermore, demographic data (professional group, qualifications, length of employment, working hours) and information on the current handover process (number of patients, handover duration, handover location, handover frequency) were collected.
Prior to data collection, a positive ethics vote was obtained, along with approvals from the works council, the data protection officer, and the hospital’s nursing management. Pre-tests were conducted with nine nursing staff members from four wards, followed by expert interviews. After integrating the questions “In your opinion, has handover quality changed with electronic documentation compared to paper-based documentation?”, and “If so, how has handover quality in electronic documentation changed from your perspective?” into the survey instrument at time point t1, no further adjustments were required.
Only nurses working in a general ward at Helios Klinikum München West with a completed professional nursing qualification were included in the study. For approval-related and methodological reasons, a between-subject design was used, meaning different participants were surveyed at each data collection point, and those who took part in the first survey did not necessarily participate in the second. Recruitment was conducted through written information provided to ward managers, along with the distribution of 260 information sheets and questionnaires across 13 wards. Participation was voluntary, anonymous, and available for three weeks at each data collection point. Nurses consented to participate by placing their completed questionnaires into sealed return boxes at each ward’s central station. No financial compensation was provided.
Data analysis
Data analysis was conducted using IBM SPSS Statistics (Version 28.0) and JASP (Version 0.17.1.0). The alpha level for statistical analyses was set at α=.05 (two-tailed significance). In addition to the descriptive analysis of social variables, relevant pre-post comparisons were performed using inferential statistics, including the chi-square test, Mann-Whitney U test, and independent samples t-test. For analyses at the total score and subscale levels, the negatively worded items F14, F15, and F16 from the German version of the Handover Evaluation Scale were recoded.
Results
Sociodemographic and handover-specific data
The total sample size was n=176. The adjusted response rate was 30.8% (n=80) at t0 and 36.9% (n=96) at t1. Since the response rates at both time points were based on independent samples, the use of an independent samples t-test was justified. The analysis of sociodemographic and handover-specific variables revealed no statistically significant differences (p>.05) between t0 and t1 (see Table 2 [Tab. 2]).
Table 2: Results of sociodemographic and handover-specific variables (own representation)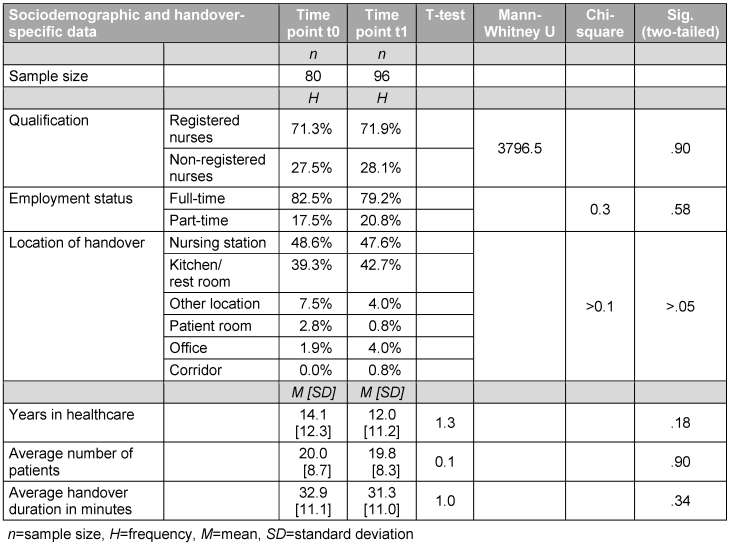
Change in handover quality between time points t0 and t1
Comparisons between time points t0 and t1 are made based on the three subscales of the German translation of the Handover Evaluation (see Table 3 [Tab. 3], Figure 1 [Fig. 1], Figure 2 [Fig. 2] and Figure 3 [Fig. 3]).
Table 3: Results of the assessment of handover quality (own representation)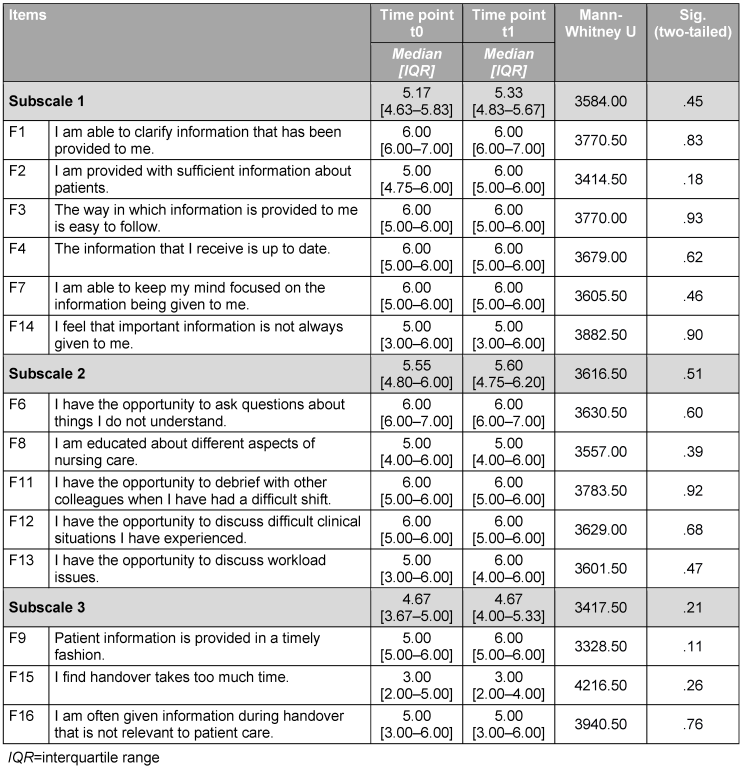
Figure 1: Assessment of handover quality. Box and whisker plot of subscale 1 (quality of information) of the Handover Evaluation Scale. Own representation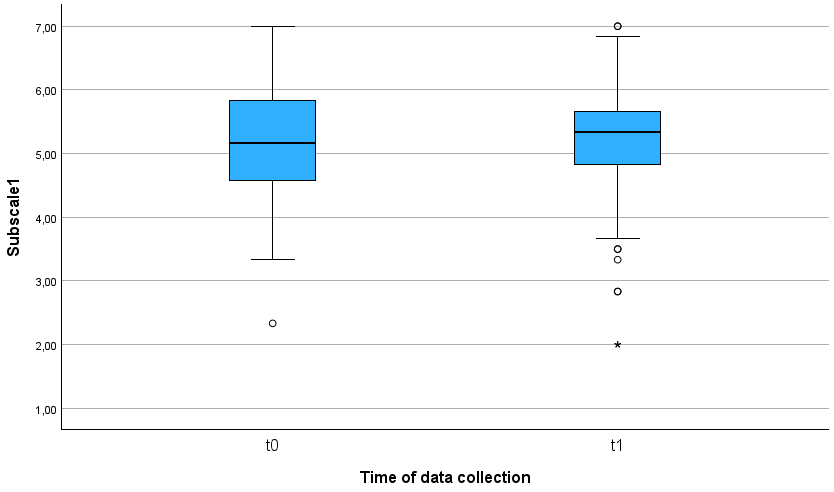
Figure 2: Assessment of handover quality. Box and whisker plot of subscale 2 (interaction and support) of the Handover Evaluation Scale. Own representation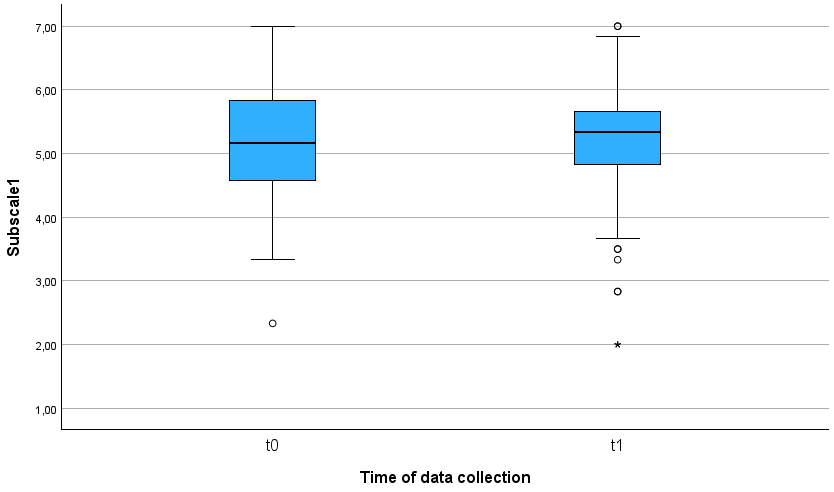
Figure 3: Assessment of handover quality. Box and whisker plot of subscale 3 (efficiency) of the Handover Evaluation Scale. Own representation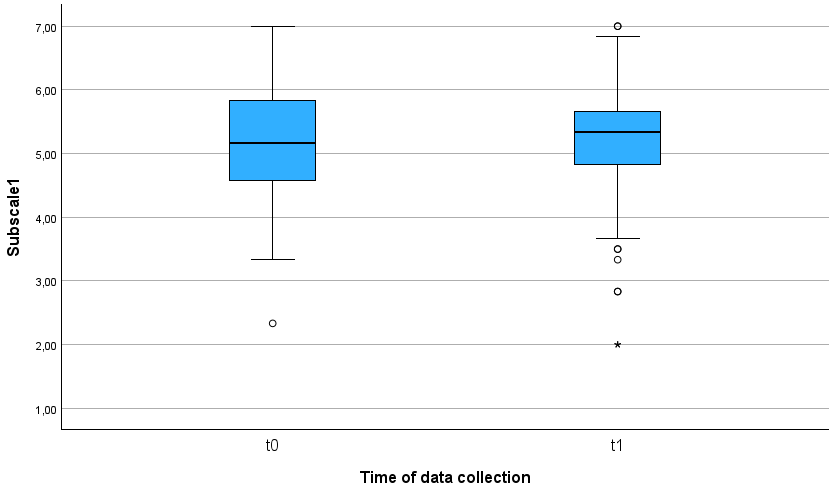
The analysis of the individual subscales shows no statistically significant results (subscale 1 p=.45, subscale 2 p=.51, subscale 3 p=.21). However, a slight trend toward improvement is observed in subscale 1 (quality of information), subscale 2 (interaction and support), and subscale 3 (efficiency). In contrast, the descriptive results for item F25 (Question 25 – In your opinion, has handover quality changed with electronic documentation compared to paper-based documentation?) at time point t1 show that 54.7% of respondents (n=52) observed a change in handover quality after the implementation of electronic documentation. In contrast, 25.3% of respondents (n=24) reported no change. Among those who reported a change in handover quality, 11.1% (n=6) rated it much worse, 31.5% (n=17) rated it worse, 22.2% (n=12) rated it about the same, 33.3% (n=18) rated it better, and 1.9% (n=1) rated it much better.
Discussion
Interpretation and discussion
This study shows that no statistically significant improvement in handover quality was observed after the implementation of electronic nursing documentation. While O’Connell et al. [3] arrived at a more positive assessment of information quality and efficiency, these findings could not be confirmed to the same extent in this study. Notably, interaction and support were rated slightly lower in O’Connell et al.’s results [3]. However, their findings concerning time-consuming handovers, the absence of relevant information, and the transmission of irrelevant patient information largely align with the data from this study [3]. Randell et al. [4] emphasize that electronic nursing documentation systems can alter the way information is exchanged and evaluated between shifts. In contrast to Randell et al. [4], this study found no statistically significant effects, which warrants further investigation. Additionally, the descriptive result for item V25a (improvement or deterioration in handover quality after the implementation of electronic documentation) at time point t1 is noteworthy. The majority of respondents subjectively reported a deterioration in handover quality following the implementation of electronic nursing documentation. The reasons why participants believed the quality declined were not explored.
Possible reasons for the lack of statistical significance and the subjective assessments from respondents may stem from inherent challenges associated with digitalization. The transition from paper-based to electronic nursing documentation could have influenced the results [1], [16]. For the target sample, this shift represented an innovation without prior experience, as the nursing staff had previously worked exclusively with paper-based documentation and had limited familiarity with digital systems. Since this transition fundamentally altered established workflows, uncertainties among the nursing staff may have affected their evaluation of handover quality [12]. Alternatively, it is possible that the needs of the nursing staff in communication and coordination processes were not adequately supported by the electronic nursing documentation system. Kutney-Lee et al. emphasize that the benefits of electronic documentation systems can only be realized when context is considered [17]. Additionally, methodological limitations – such as the insufficient validity of the questionnaire or inadequate consideration of contextual factors – may have negatively affected the implementation and use of electronic nursing documentation in daily practice [17]. A critical analysis of the results suggests that the lack of improvement could also be attributed to technical difficulties, insufficient training, or other obstacles. It raises the question of whether the technology itself was ineffective, or if its implementation could have been better designed. At the time of the second data collection in February 2022, it is possible that the electronic nursing documentation system had not yet been fully integrated into daily routines, or that the training was insufficient to provide the nursing staff with the necessary confidence to use the new system effectively [12]. In conclusion, it is evident that the successful implementation of electronic documentation systems depends not only on technical execution but also on considering the specific needs of nursing staff and nursing practices.
Limitations
The significance of the study results is limited by overlapping effects, the sample, response tendencies, and the questionnaire. The data were collected in July 2021 and February 2022, a period significantly influenced by the COVID-19 pandemic and its associated impacts. It is likely that responses, particularly regarding perceived interaction and support, were affected by these circumstances, and there is no guarantee that the responses accurately reflect the participants’ actual perceptions. Regarding the non-systematic recruitment of study participants, there is a possibility that individuals participated primarily out of personal interest and initiative. Due to the pre-post design with an independent sample, it was not possible to capture changes in the evaluation of handover quality over time [18]. The frequency distributions of the negatively worded items F14, F15, and F16 suggest an acquiescence bias. This tendency to agree with statements regardless of content indicates that the respondents often rated the statements independently of their actual meaning. Possible reasons for this include the design and length of the questionnaire, limited time resources, and respondent uncertainty. Furthermore, all responses in the written survey were based on self-assessments, which could have been influenced by social desirability bias. A critical issue is that the German version of the Handover Evaluation Scale, in its current form, does not fully capture all relevant dimensions of handover quality, as intended by O’Connell et al. [3]. Due to insufficient construct validity, several adjustments are necessary for the German version.
Implications
The results of this study suggest that the introduction of electronic nursing documentation did not lead to a statistically significant improvement in handover quality. However, it is crucial to distinguish between statistical significance and clinical relevance. Even in the absence of statistical significance, electronic nursing documentation may still offer practical benefits in daily nursing routines and positively influence care quality. This highlights the need for further research and optimization in the implementation and use of digital systems.
Future research should focus on minimizing overlapping effects, ensuring systematic participant recruitment, and utilizing a connected sample. This approach could improve the comparability of results and provide deeper insights into the impact of electronic nursing documentation on handover quality. As previously highlighted by O’Connell et al., there is a clear need to optimize the nursing handover process [3]. Developing standardized guidelines to enhance this process would be valuable. Reducing irrelevant information and emphasizing key patient details may help improve the efficiency of handovers and increase their consistency and reliability [15]. The introduction of checklists and standardized protocols, as recommended in related studies, could contribute to higher handover quality by ensuring that all relevant information is considered. In addition, regular training sessions for nursing staff should be implemented to enhance their proficiency in using electronic nursing documentation and optimizing the handover process. Furthermore, integrating the Clinical Adoption Meta-Model [19] could help address not only technological but also social and organizational factors during the implementation of new technologies in healthcare, ultimately improving the overall adoption and effectiveness of digital systems.
Conclusion
The handover of patient information is a crucial routine process in nursing. This study shows that, contrary to literary assumptions, no statistically significant improvement in handover quality was observed after the implementation of electronic nursing documentation. Hospitals that adopt digital documentation systems should always focus on transformation and process management. Additionally, optimizing and standardizing the handover process and integrating the Clinical Adoption Meta-Model can be beneficial.
Notes
Ethical approval
Interdisciplinary Ethics Committee for Research of Katholische Stiftungshochschule München, Chair: Prof. Dr. Constanze Giese, Date of result submission: 02.07.2021.
Author contributions
- SS: Conception and design of the study, data collection, data analysis, interpretation, drafting of the manuscript
- DF: Conception of the study, manuscript revision
- BR: Conception of the study, manuscript revision
All authors have approved the manuscript in its submitted form and take responsibility for the scientific integrity of the work.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank O’Connell et al. for providing the English-language Handover Evaluation Scale. They also wish to thank for the provision of the unpublished German translation of the Handover Evaluation Scale.
References
[1] Fachinger U, Mähs M. Digitalisierung und Pflege. In: Klauber J, Geraedts M, Friedrich J, Wasem J, editors. Krankenhaus-Report 2019: Das digitale Krankenhaus. Berlin, Heidelberg: Springer-Verlag; 2019. p. 115-28. DOI: 10.1007/978-3-662-58225-1[2] Rösler U, Schmidt K, Merda M, Melzer M. Digitalisierung in der Pflege: Wie intelligente Technologien die Arbeit professionell Pflegender verändern. Berlin: Geschäftsstelle der Initiative Neue Qualität der Arbeit; 2018. p. 5-31.
[3] O’Connell B, Macdonald K, Kelly C. Nursing handover: It’s time for a change. Contemp Nurse. 2008 Aug;30(1):2-11. DOI: 10.5172/conu.673.30.1.2
[4] Randell R, Wilson S, Woodward P. The importance of the verbal shift handover report: a multi-site case study. Int J Med Inform. 2011 Nov;80(11):803-12. DOI: 10.1016/j.ijmedinf.2011.08.006
[5] Flemming D, Hübner U. How to improve change of shift handovers and collaborative grounding and what role does the electronic patient record system play? Results of a systematic literature review. Int J Med Inform. 2013 Jul;82(7):580-92. DOI: 10.1016/j.ijmedinf.2013.03.004
[6] Deutsche Krankenhausgesellschaft. Hinweise der Deutschen Krankenhausgesellschaft für die Ausgestaltung der Förderung von Digitalisierung im Krankenhaus nach dem Krankenhaus-Zukunfts-Gesetz (KHZG). Berlin: Deutsche Krankenhausgesellschaft e. V.; 2020. p. 4-24.
[7] Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inform. 2008 May;77(5):291-304. DOI: 10.1016/j.ijmedinf.2007.09.001
[8] Ihlebæk HM. Lost in translation – Silent reporting and electronic patient records in nursing handovers: An ethnographic study. Int J Nurs Stud. 2020 Sep;109:103636. DOI: 10.1016/j.ijnurstu.2020.103636
[9] Kruse CS, Beane A. Health Information Technology Continues to Show Positive Effect on Medical Outcomes: Systematic Review. J Med Internet Res. 2018 Feb;20(2):e41. DOI: 10.2196/jmir.8793
[10] Uslu A, Stausberg J. Value of the Electronic Medical Record for Hospital Care: Update From the Literature. J Med Internet Res. 2021 Dec;23(12):e26323. DOI: 10.2196/26323
[11] Muinga N, Abejirinde IO, Paton C, English M, Zweekhorst M. Designing paper-based records to improve the quality of nursing documentation in hospitals: A scoping review. J Clin Nurs. 2021 Jan;30(1-2):56-71. DOI: 10.1111/jocn.15545
[12] Lauterbach A. „Das stimmt nicht, was da steht“ – Zur Qualität IT-basierter Pflegedokumentationen. PrInterNet – Zeitschrift für Pflegewissenschaft. 2009;(02/09):95-104.
[13] Karsten T, Koopmans J, Martens C, Steinmaier V. Unveröffentlichte deutsche Übersetzung der Handover Evaluation Scale. München: Katholische Stiftungshochschule München; 2014.
[14] Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005 Mar-Apr;8(2):94-104. DOI: 10.1111/j.1524-4733.2005.04054.x
[15] O’Connell B, Ockerby C, Hawkins M. Construct validity and reliability of the Handover Evaluation Scale. J Clin Nurs. 2014 Feb;23(3-4):560-70. DOI: 10.1111/jocn.12189
[16] Wasem J. Digitalisierung im Krankenhaus – eine Einführung. In: Klauber J, Geraedts M, Friedrich J, Wasem J, editors. Krankenhaus-Report 2019: Das digitale Krankenhaus. Berlin, Heidelberg: Springer-Verlag; 2019. p. XIII-XV. DOI: 10.1007/978-3-662-58225-1
[17] Kutney-Lee A, Sloane DM, Bowles KH, Burns LR, Aiken LH. Electronic Health Record Adoption and Nurse Reports of Usability and Quality of Care: The Role of Work Environment. Appl Clin Inform. 2019 Jan;10(1):129-139. DOI: 10.1055/s-0039-1678551
[18] Tuna R, Dalli B. The Turkish version of the Handover Evaluation Scale: A validity and reliability study. Int J Nurs Pract. 2019 Dec;25(6):e12787. DOI: 10.1111/ijn.12787
[19] Price M. Clinical Adoption Meta-Model. Chapter 4. In: Lau F, Kuziemsky C, editors. Handbook of eHealth Evaluation: An Evidence-based Approach. Victoria (BC): University of Victoria; 2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK481589/




