Cognitive assistive technologies for degenerative diseases and related evaluation methods: A scoping review
Robin Grashof 1Myriam Lipprandt 2
Bernhard Breil 1
1 Faculty of Health Care, Hochschule Niederrhein University of Applied Sciences, Krefeld, Germany
2 Institute of Medical Informatics, Medical Faculty of RWTH Aachen University, Aachen, Germany
Abstract
Assistive technologies (ATs) are crucial for people with degenerative diseases that affect cognitive functions. To date, no comprehensive review has systematically examined these technologies and their evaluation methods. To outline the current state of research, we conducted a scoping review on cognitive ATs that provide direct assistance. From an initial pool of 107 review articles identified in Web of Science and other sources over the last five years we selected ten for further analysis. To enhance clarity and interpretability, the findings were organized into thematic categories, distinguishing types of assistive technologies as well as evaluation approaches used across studies.
The articles included focus primarily on ATs for people with dementia. The majority of systems are wearable, prioritizing biometric and motion data, with a preference for mobile devices over stationary solutions. While many ATs address physiological concerns such as falls, they generally neglect psychiatric symptoms, although social robots help to improve engagement and emotions. Evaluation studies predominantly rely on behavioral assessments instead of self-reported outcomes often with limited sample sizes.
It’s important to involve secondary users, such as family and professional caregivers, and to consider the compatibility of ATs with users’ cognitive and physical abilities. Future research should incorporate systematic analyses and case studies to enhance the methodological rigor of evaluation studies, particularly regarding key outcomes, sample sizes, and study designs.
Keywords
degenerative disease, assistive technology, evaluation methods, health care
Introduction
Cognitive symptoms are a hallmark of various chronic diseases. Patients living with chronic diseases like dementia, mild cognitive impairment, Parkinson disease or multiple sclerosis may experience challenges in multiple domains like memory, delirium, planning, learning, language, mood changes or social cognition [1], [2], [3], [4]. In light of technological advancements assistive technologies (AT) for clinical applications have gained increasing attention in recent years. According to the World Health Organization, an AT is the application of organized knowledge and skills related to assistive products, including systems and services [5]. They call several application fields for ATs like education, work, (mental) health, physical activities and leisure, everyday activities and social relationships [6]. While some of the systems are developed to facilitate the everyday life of caregivers and other medical professionals [7] there are ATs for the concerned people themselves [8].
Lopresti and Bodine [9] gave an overview about AT for cognitive disabilities and important barriers due to design process, published in 2008, Thordardottir et al. [10] examined the acceptance of AT for cognitive impairments in 2019. A current review from Lee-Chong et al. [11] displayed AT focusing on dementia and cognitive impairment care. Ebuenyi et al. [12] gave a systematic overview about current AT for people with psychosocial disabilities but they excluded papers concerning people with cognitive disabilities.
Objective
Numerous review papers have been published which examine primary articles in the context of ATs for degenerative diseases with a range of focal areas. The objective of this paper is to provide an overview of the research focus on cognitive ATs for clinical applications guided by the PRISMA-ScR framework [13], identifying well-explored areas as well as existing research gaps. Specifically, we examine the available systems and the evaluation methods applied in these studies.
Methods
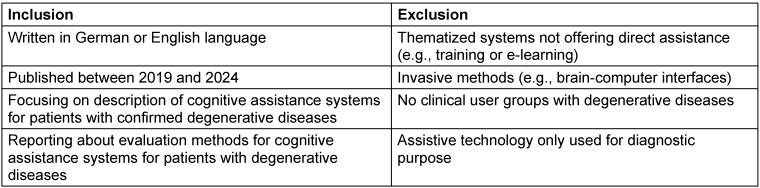
Eligibility criteria
Articles were eligible for inclusion if they were open access reviews published in the last five years and focused on the description of cognitive assistance systems for patients with confirmed degenerative diseases or reported about evaluation methods for these systems. We excluded articles concerning systems not offering direct assistance, invasive methods, no clinical user groups or ATs only offering diagnostic functionalities. Eligibility criteria are displayed in Table 1 [Tab. 1]. We did not register a review protocol.
Search strategy
We conducted a literature search in Web of Science on 28.08.2024. The search string is displayed in Figure 1 [Fig. 1]. We also included six articles from other sources, derived from the authors’ professional expertise, reference lists of prior publications, institutional journal club discussions, and scholarly exchanges with peers in the field. These articles were included to ensure that key content perspectives were covered.
Figure 1: Utilized search string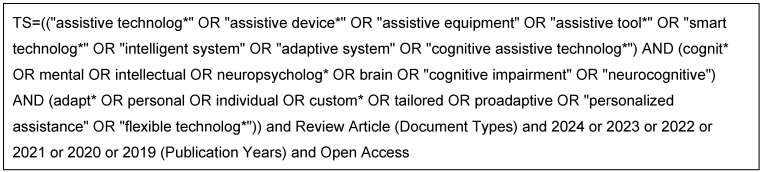
Selection and data collection process
Articles were screened by title and abstract and then in a second iteration we had a deeper look into the articles. The screening and examination processes were conducted by one author (RG). Where ambiguities or uncertainties arose, a second reviewer was involved to validate the assessment. All included articles were analyzed once each with a focus on AT and evaluation methods, marked in different colors in the documents. At next, relevant information on AT and evaluation methods from each article was collected in a separate document. Data extraction was conducted by one author (RG). No specific data extraction tool was utilized.
Data items
We abstracted data on article characteristics (e.g., included articles, focus, psychological aspects), AT characteristics (e.g., physical properties, functionalities, target groups, mobility, deployment context), evaluation methods (e.g., outcome measures, applied methods, target groups), addressed diseases (e.g., Alzheimer disease, Parkinson disease, multiple sclerosis) and to what extent AI was mentioned and in what context.
Results
Study selection
Initially, 107 articles were identified without any duplicates. After title and abstract screening, 35 articles (33%) remained. Subsequently, 25 articles were removed after reading the full text, to extract ten articles (9%) from our database. Study selection is displayed in Figure 2 [Fig. 2].
Figure 2: Flowchart of study selection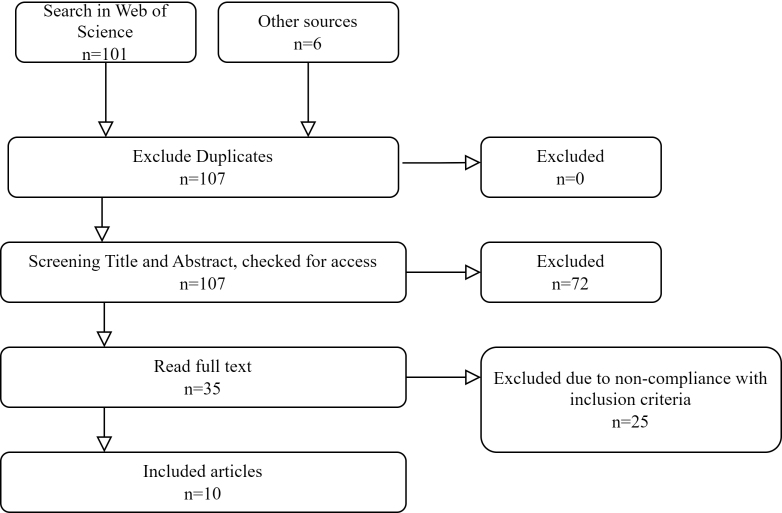
The other sources category includes materials identified through prior knowledge, journal club debates within the institution, professional experience, and consultations with other field researchers.
Characteristics of included articles
Most articles provided clear descriptions of their search strategies and inclusion criteria, yet only a few explicitly reported on the methodological quality of the primary studies. Furthermore, only a minority applied established frameworks or appraisal tools to guide the synthesis process. As a result, the overall quality and comparability of findings across reviews are heterogeneous, which should be considered when interpreting the results presented below. Further characteristics of the articles are shown in Table 2 [Tab. 2]. Although our search covered a broad range of terms, the majority of identified articles focus on AT for elderly and people with dementias. As some articles do not clearly distinguish between Alzheimer disease and dementia, the more general term “dementia” will be used in the subsequent section. Smart devices using artificial intelligence (AI) are mentioned in seven of the ten included articles, but aren’t examined separately. Consequently, the matter will not be pursued further.
Table 2: Characteristics of included articles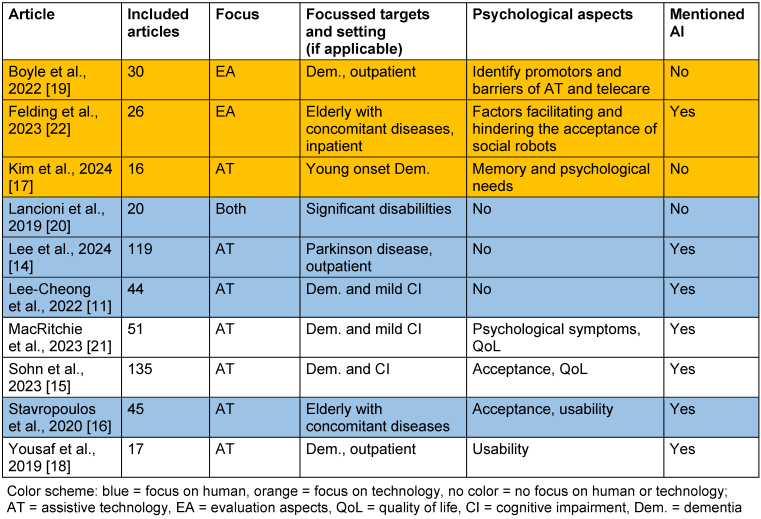
Assistive technologies
Across all ten included articles, a wide range of ATs was identified, primary targeting individuals with dementia, cognitive impairment, or Parkinson disease. To improve clarity and comparability, the ATs were heuristically categorized according to their functional characteristics, degree of mobility, and typical deployment context (see Table 3 [Tab. 3]), whereas there is also potential for overlap between the categories.
Table 3: Categorized AT and deployment contexts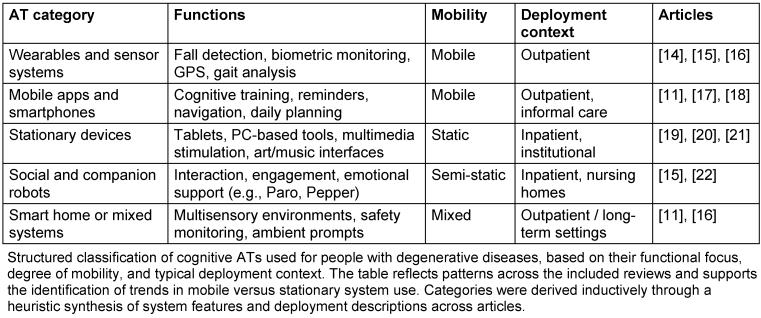
“Wearables and sensor systems” were among the most frequently discussed technologies. These include smart textiles, GPS trackers, and biometric sensors capable of monitoring movement patterns, physiological data, or spatial orientation. Such systems are predominantly used for fall detection, emergency response, and gait analysis [14], [15], [16]. Several studies described the use of “mobile apps and smartphones”, often focusing on cognitive training, daily planning, navigation support, and caregiver communication. These apps are typically designed for patients with early-stage dementia or mild cognitive impairment and are accessible in outpatient or home environments [11], [17], [18]. A third category comprises “stationary devices”, including tablet-based memory aids, multimedia tools for reminiscence or emotional expression, and interactive systems used in structured settings such as care facilities. These systems often support psychosocial engagement and were mostly designed for supervised or semi-autonomous use [19], [20], [21]. “Social and companion robots” represent a distinct group of ATs with a focus on interaction and emotional stimulation. These robots – both humanoid and zoomorphic – are typically deployed in institutional settings to promote engagement, alleviate loneliness or support therapeutic routines. Articles reported their potential to evoke emotional responses and enhance quality of life, although their acceptance may vary considerably [15], [22]. Finally, “smart home or mixed systems” integrate multiple sensors, ambient prompts, and automation technologies. These systems aim to support safety, autonomy, and daily functioning in home environments. Features include medication reminders, environmental controls, and adaptive lighting or audio feedback [11], [16].
This categorization highlights a trend towards mobile and personalized systems, often targeting specific symptoms (e.g., impaired memory or fall risk) and settings (e.g., outpatient care or long-term living). Complex or costly systems tended to be static and institution-based, whereas simpler, app-based solutions were more common in home care settings.
Applied evaluation methods
The included reviews described a broad range of evaluation strategies used to assess cognitive ATs for individuals with degenerative diseases across all included articles. To structure the diversity of approaches, we classified the evaluation focus into six heuristic categories: usability and acceptance, effectiveness and impact, feasibility, technical safety and reliability, ethical and emotional aspects, and target group-specific fit (see Table 4 [Tab. 4]). “Usability and acceptance” is the most frequently addressed evaluation category. Articles often focused on user experience, perceived usefulness, and ease of use – particularly in relation to social robots and mobile applications. Several evaluations employed standardized frameworks such as the ALMERE model (special focus in Felding et al. [22]), standardized scales or used structured interviews with both primary users (patients) and secondary users (caregivers) to assess acceptance and engagement [15], [16], [19], [22]. “Effectiveness and impact” were measured through behavioral observations and outcome indicators such as mood, social interaction, and cognitive activation. These assessments were applied in the context of art-based interventions, memory aids, or stimulation systems [17], [20], [21]. “Feasibility” was addressed primarily by MacRitchie et al. [21], who examined the practical implementation of art-based technologies for people with cognitive impairment. Key aspects of observational feasibility assessments included setup effort, sustained use, and the need for caregiver support. “Technical safety and reliability” were examined particularly in mobile and sensor-based systems. Evaluations included the frequency of system failures, quality of sensor data, and reliability of emergency call features [11], [14], [19]. “Ethical and emotional aspects” played a role in studies evaluating technology-related anxiety, cultural barriers, or fears of dehumanization. These evaluations used qualitative methods and involved both users and professionals to capture nuanced attitudes and emotional reactions [19], [22]. Finally, some studies addressed “target group-specific fit”, highlighting the importance of aligning AT design with individual cognitive, emotional, and sensory capabilities. Co-design approaches and proxy assessments by caregivers were suggested to ensure that technologies remain usable even in progressive disease stages [11], [19]. Across studies, a notable trend was the involvement of not only patients but also (professional) caregivers and family members in the evaluation process. Mixed-method designs combining quantitative and qualitative data were common, particularly in socially complex environments like nursing homes.
Table 4: Evaluation categories and applied methods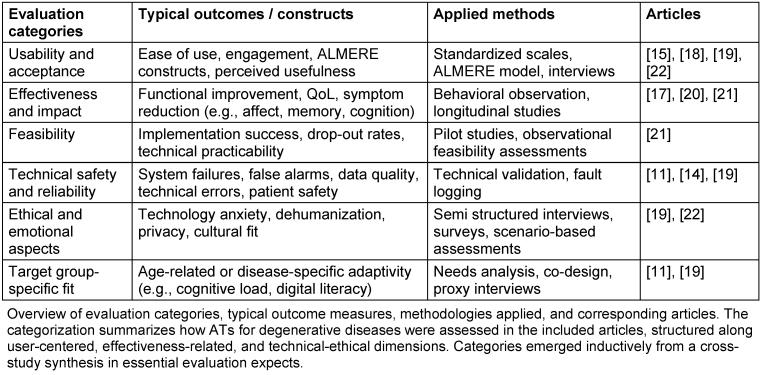
Discussion
Summary and interpretation
We gave a scoping overview about review articles concerning existing cognitive ATs for people with degenerative diseases. Most of our included papers focused on dementia, while Parkinson disease and other cognitive impairments were less frequently addressed. The present study adopted an inducible categorization approach for ATs as a methodology that has been employed in other review articles concerning ATs for dementia. We proposed five categories: Wearables and Sensor Systems, Mobile Apps and Smartphones, Stationary Devices, Social and Companion Robots and Smart Home or Mixed Systems. However, while there is some resemblance, AT categories in review articles are not identical. For example, Ma et al. focused on outcome measures [23], while Sriram et al. categorized for main use and subdivided for AT type [24]. Concerning our findings, two general categories can be distinguished: Firstly, there are static and expensive systems, which are mostly found in inpatient settings. One system can be used by multiple users, with supervision being provided by caregivers in some cases. Secondly, there are proportionally mobile and inexpensive systems designed for a single long-term user without autonomous usage.
Many described systems used wearables to provide assistance measure sensor data in one device, whereas most used data were biometric measures and movement data. Some systems used existing devices like smartphones. It is noticeable that mobile devices are used more often than permanently installed components such as PCs or stationary cameras. Physiological issues (e.g., falls, important biomarkers) are more often addressed than psychiatric symptoms. This aligns with recent findings that emphasize the increasing role of mobile, decentralized ATs in dementia care, particularly for physiological monitoring tasks such as fall detection and movement tracking [25]. However social robots seem to close this gap by enhancing engagement, providing entertainment, and bringing positive emotions. While Hung et al. [26] stated that more attention to the clinical needs of dementia patients is needed in a review about the social robot Paro in 2019, our evidence suggests such a trend in the subsequent years.
The reported evaluation processes often used behavioral assessments rather than standardized scales. Acceptance was the most mentioned psychological outcome measure. Sample sizes varied, but were predominantly small, which could be explained by the high effort for recruitment as well as for patients and as test subjects. These observations align with recent findings that small and heterogeneous sample sizes limit generalizability in AT research [27]. It seems important to involve potential secondary users like (caregiving) family members or professional caregivers, especially when the patient (as primary user) receives outpatient care or lives in a retirement home with inpatient care. This is supported by previous research emphasizing the role of caregivers in the successful adoption, adaptation, and sustained use of ATs [24]. Evaluators also need to ensure that ATs match with users’ health-specific and age-related capabilities and requirements (e.g., impaired cognitive processing, restricted mobility or concurrent neuropsychiatric symptoms as well as poor digital literacy). Evaluations that include user-centered adaptations, like simplified interfaces, memory support tools, or voice-controlled functions, are associated with higher acceptance and better task performance as stated in current literature [10], [28]. These findings highlight that cognitive ATs must be context-specific and cognitive accessible to in order to guarantee that the complete potential of an AT is realized.
Limitations and perspective
The screening process of articles and their subsequent examination was conducted by a single author, with the second author providing support due to uncertainties. The quality of the methodological approach and the objectivity of the article selection process could have been enhanced if the process had been conducted independently by at least two authors. As we focused on review articles findable in Web of Science, the displayed ATs probably do not cover all existing technologies in this field. The limited financial resources available to patients, in conjunction with the inadequacy of health insurance systems in terms of financial coverage, results in restricted access to ATs for many individuals. Together with the recent advent of ATs themselves and the limitation to review articles in one database, this may result in the paucity of found articles on ATs. The found evaluation methods are mostly psychological constructs. To get a better understanding about how to a plan an evaluation study, which constructs are most important, which sample sizes or which time period for longitudinal designs, a systematic analysis including case studies would be necessary. Notably, three ([11], [15], [16]) of the ten included articles were added manually rather than identified through database search, even though they fit our eligibility criteria very well. It is possible that the terminology in this new field of research is still too inconsistent. Across the included studies, terms such as “technology”, “device”, “dementia”, and “pwd” (people with dementia) appeared with notable frequency, reflecting a terminological overlap within the field. This suggests a predominant focus on dementia-related interventions and highlights the lack of terminological standardization in AT research. Finally, AI as an emerging area of technology was mentioned in most articles, but did not have any particular significance. This may change in the coming years, influencing AT to become smarter and more personalized in healthcare, as the implementation of AI in personalized social robots is an emerging topic of interest [26], [29].
Conclusion
Across the articles, a common thread is the integration of ATs to enhance autonomy, safety and engagement among elderly individuals. While wearables, smart home solutions, and robotics show great promise, challenges remain in terms of user adaptation, personalization, and acceptance. Future research should focus on optimizing these technologies to ensure they remain accessible, effective, and user-friendly for aging populations.
Notes
Funding
This work has been funded by the Ministry of Culture and Science of the State of North Rhine-Westphalia via the Profilbildung 2022 project Zentrum Assistive Technologien (ZAT) Rhein-Ruhr (PB22-076C).
Competing interests
The authors declare that they have no competing interests.
Informed consent
All persons included in this project have given their informed consent.
Authors’ contributions
RG and BB designed the study and search strategies. RG performed the literature research and drafted the manuscript. BB supervised manuscript drafting. BB and ML revised the manuscript. All authors read and approved the final manuscript.
References
[1] Hiu SKW, Bigirumurame T, Kunonga P, Bryant A, Pillai M. Neuropsychiatric Inventory domains cluster into neuropsychiatric syndromes in Alzheimer’s disease: A systematic review and meta-analysis. Brain Behav. 2022 Sep;12(9):e2734. DOI: 10.1002/brb3.2734[2] Dhakal A, Bobrin BD. Cognitive Deficits. In: StatPearls. Treasure Island (FL): StatPearls Publishing. [Last updated 2023 Feb 14]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559052/
[3] Benedict RHB, Amato MP, DeLuca J, Geurts JJG. Cognitive impairment in multiple sclerosis: clinical management, MRI, and therapeutic avenues. Lancet Neurol. 2020 Oct;19(10):860-71. DOI: 10.1016/S1474-4422(20)30277-5
[4] Sauerbier A, Jenner P, Todorova A, Chaudhuri KR. Non motor subtypes and Parkinson’s disease. Parkinsonism Relat Disord. 2016 Jan;22 Suppl 1:S41-6. DOI: 10.1016/j.parkreldis.2015.09.027
[5] World Health Organization; USAID; International Disability Alliance. Priority assistive products list: improving access to assistive technology for everyone, everywhere. WHO/EMP/PHI/2016.01. WHO; 2016. Available from: https://iris.who.int/handle/10665/207694
[6] World Health Organization; United Nations Children’s Fund. Global Report on Assistive Technology. Geneva: WHO; 2022. ISBN: 9789240049451. Available from: https://www.who.int/publications/i/item/9789240049451
[7] Choi UY, Patterson P, Chinho N. Reducing the Burdens of Paid Caregivers of Older Adults by Using Assistive Technology: A Scoping Review. West J Nurs Res. 2024 Apr;46(4):315-26. DOI: 10.1177/01939459241234233
[8] Cooper RA, Dicianno BE, Brewer B, LoPresti E, Ding D, Simpson R, Grindle G, Wang H. A perspective on intelligent devices and environments in medical rehabilitation. Med Eng Phys. 2008 Dec;30(10):1387-98. DOI: 10.1016/j.medengphy.2008.09.003
[9] LoPresti EF, Bodine C, Lewis C. Assistive technology for cognition. IEEE Eng Med Biol Mag. 2008;27(2):29-39. DOI: 10.1109/EMB.2007.907396
[10] Thordardottir B, Malmgren Fänge A, Lethin C, Rodriguez Gatta D, Chiatti C. Acceptance and Use of Innovative Assistive Technologies among People with Cognitive Impairment and Their Caregivers: A Systematic Review. Biomed Res Int. 2019;2019:9196729. DOI: 10.1155/2019/9196729
[11] Lee-Cheong S, Amanullah S, Jardine M. New assistive technologies in dementia and mild cognitive impairment care: A PubMed review. Asian J Psychiatr. 2022 Jul;73:103135. DOI: 10.1016/j.ajp.2022.103135
[12] Ebuenyi ID, Flocks-Monaghan C, Rai SS, Vries R, Bhuyan SS, Pearlman J, Jones N. Use of Assistive Technology for Persons with Psychosocial Disability: Systematic Review. JMIR Rehabil Assist Technol. 2023 Nov;10:e49750. DOI: 10.2196/49750
[13] Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018 Oct;169(7):467-73. DOI: 10.7326/M18-0850
[14] Lee DH, Woo BS, Park YH, Lee JH. General Treatments Promoting Independent Living in Parkinson's Patients and Physical Therapy Approaches for Improving Gait-A Comprehensive Review. Medicina (Kaunas). 2024 Apr;60(5):711. DOI: 10.3390/medicina60050711
[15] Sohn M, Yang J, Sohn J, Lee JH. Digital healthcare for dementia and cognitive impairment: A scoping review. Int J Nurs Stud. 2023 Apr;140:104413. DOI: 10.1016/j.ijnurstu.2022.104413
[16] Stavropoulos TG, Papastergiou A, Mpaltadoros L, Nikolopoulos S, Kompatsiaris I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors (Basel). 2020 May;20(10):2826. DOI: 10.3390/s20102826
[17] Kim I, Yang Y, Cheon H, Kim J, Song JA. Non-pharmacological interventions for people living with young-onset dementia and their carers: A scoping review focussing on the support of participants' needs. J Psychiatr Ment Health Nurs. 2024 Feb;31(1):14-30. DOI: 10.1111/jpm.12954
[18] Yousaf K, Mehmood Z, Saba T, Rehman A, Munshi AM, Alharbey R, Rashid M. Mobile-Health Applications for the Efficient Delivery of Health Care Facility to People with Dementia (PwD) and Support to Their Carers: A Survey. Biomed Res Int. 2019;2019:7151475. DOI: 10.1155/2019/7151475
[19] Boyle LD, Husebo BS, Vislapuu M. Promotors and barriers to the implementation and adoption of assistive technology and telecare for people with dementia and their caregivers: a systematic review of the literature. BMC Health Serv Res. 2022 Dec;22(1):1573. DOI: 10.1186/s12913-022-08968-2
[20] Lancioni GE, Olivetti Belardinelli M, Singh NN, O’Reilly MF, Sigafoos J, Alberti G. Recent Technology-Aided Programs to Support Adaptive Responses, Functional Activities, and Leisure and Communication in People With Significant Disabilities. Front Neurol. 2019;10:643. DOI: 10.3389/fneur.2019.00643
[21] MacRitchie J, Floridou GA, Christensen J, Timmers R, de Witte L. The use of technology for arts-based activities in older adults living with mild cognitive impairment or dementia: A scoping review. Dementia (London). 2023 Jan;22(1):252-80. DOI: 10.1177/14713012221127359
[22] Felding SA, Koh WQ, Teupen S, Budak KB, Laporte Uribe F, Roes M. A Scoping Review Using the Almere Model to Understand Factors Facilitating and Hindering the Acceptance of Social Robots in Nursing Homes. International Journal of Social Robotics. 2023;15(7):1115-53. DOI: 10.1007/s12369-023-01012-1
[23] Ma Y, Nordberg OE, Hubbers J, Zhang Y, Rongve A, Bachinski M, Fjeld M. Bridging the Gap: Advancements in Technology to Support Dementia Care – A Scoping Review [Preprint]. arXiv. 2024. DOI: 10.48550/arXiv.2404.09685
[24] Sriram V, Jenkinson C, Peters M. Informal carers’ experience of assistive technology use in dementia care at home: a systematic review. BMC Geriatr. 2019 Jun;19(1):160. DOI: 10.1186/s12877-019-1169-0
[25] Pappadà A, Chattat R, Chirico I, Valente M, Ottoboni G. Assistive Technologies in Dementia Care: An Updated Analysis of the Literature. Front Psychol. 2021;12:644587. DOI: 10.3389/fpsyg.2021.644587
[26] Hung L, Liu C, Woldum E, Au-Yeung A, Berndt A, Wallsworth C, Horne N, Gregorio M, Mann J, Chaudhury H. The benefits of and barriers to using a social robot PARO in care settings: a scoping review. BMC Geriatr. 2019 Aug;19(1):232. DOI: 10.1186/s12877-019-1244-6
[27] Palmdorf S, Stark AL, Nadolny S, Eliaß G, Karlheim C, Kreisel SH, Gruschka T, Trompetter E, Dockweiler C. Technology-Assisted Home Care for People With Dementia and Their Relatives: Scoping Review. JMIR Aging. 2021 Jan;4(1):e25307. DOI: 10.2196/25307
[28] Holthe T, Halvorsrud L, Karterud D, Hoel KA, Lund A. Usability and acceptability of technology for community-dwelling older adults with mild cognitive impairment and dementia: a systematic literature review. Clin Interv Aging. 2018;13:863-86. DOI: 10.2147/CIA.S154717
[29] Lee H, Chung MA, Kim H, Nam EW. The Effect of Cognitive Function Health Care Using Artificial Intelligence Robots for Older Adults: Systematic Review and Meta-analysis. JMIR Aging. 2022 Jun;5(2):e38896. DOI: 10.2196/38896