[Adhärenz zur Hormontherapie bei Brustkrebspatientinnen: Retrospektive Datenanalyse auf Basis von Patientenakten]
Suyeon Kim 1Ye-Eun Park 1
Yura Lee 1
Jong Won Lee 2
1 Department of Information Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
2 Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Zusammenfassung
Die Therapietreue bei der adjuvanten endokrinen Therapie (AET) ist bei hormonrezeptorpositivem Brustkrebs von entscheidender Bedeutung, nimmt jedoch mit der Zeit ab. Wir haben 6.019 Patient:innen aus der Asan Biomedical Research Environment (ABLE) analysiert, die nach einer Operation eine fünfjährige Antiöstrogen-Therapie absolviert haben (2010–2018). Die Medikamenteneinnahme, gemessen anhand der Medikamentenbesitzquote (MPR), sank von 97% auf 66%, wobei besonders drastische Rückgänge in den Jahren 1–2 und 4–5 zu verzeichnen waren. Eine schlechte Adhärenz war mit einem Alter ≥50 Jahren, einer Monotherapie mit Aromatasehemmern (AIs) und dem Fehlen einer Strahlentherapie verbunden (p<0,001). Patient:innen, die von selektiven Östrogenrezeptormodulatoren (SERMs) auf AIs umstellten, zeigten die höchste Therapietreue. Diese Ergebnisse unterstreichen die Notwendigkeit einer frühzeitigen Identifizierung von Risikopatient:innen und der Entwicklung maßgeschneiderter klinischer Behandlungsstrategien. Digitale Gesundheitsinterventionen können hier Unterstützung bieten, müssen jedoch in klinischen Settings weiter validiert werden.
Schlüsselwörter
Therapietreue, adjuvante endokrine Therapie, Brustkrebs, digitale Gesundheit, Real-World Evidence
Introduction
Long-term use of adjuvant endocrine therapy (AET) reduces recurrence and improves survival in hormone receptor-positive breast cancer, but medication adherence declines over time. Real-world studies using the Medication Possession Ratio (MPR) show that up to 20% of patients discontinue AET within two years [1], and low adherence (MPR <80%) significantly increases the risk of recurrence and mortality [2], [3].
Digital health technologies such as SMS reminders, mobile apps, and AI-based behavioral interventions have been explored to improve adherence [4]. A recent review highlighted the effectiveness of these approaches in enhancing adherence to oral anticancer therapies across diverse populations [5]. As adherence patterns differ by age, treatment regimen, and duration since initiation, identifying high-risk groups and critical periods is key to guiding clinical decisions. Using real-world EHR data, this study analyzes five-year adherence trends by age and treatment type to support the development of targeted digital strategies.
Methods
Clinical data were obtained from the Asan Biomedical Research Environment (ABLE), a pseudonymized clinical data warehouse at Asan Medical Center (AMC) that provides de-identified electronic health records (EHRs). Data were extracted by a biomedical engineer and validated by a physician with a Ph.D. in biomedical informatics and clinical experience in breast cancer surgery. A total of 6,019 patients who underwent surgery (2010–2018) and completed five years of anti-estrogen therapy were included. Patients with multiple primary cancers, no surgery, stage 0 or 4 breast cancer, or follow-up intervals exceeding one year were excluded.
Medication adherence was measured using the MPR as the proportion of days covered within a year, capped at 100%. Poor adherence was defined as MPR <80%, based on commonly accepted thresholds in adherence research. Adherence was analyzed by five-year age groups and four medication categories: selective estrogen receptor modulators (SERMs), aromatase inhibitors (AIs), SERMs to AIs, and AIs to SERMs.
Statistical analyses were performed using Python 3.12.2 in Jupyter Notebook. Descriptive statistics summarized patient characteristics and adherence trends. Chi-square tests were used to compare poor (MPR <80%) and good (MPR ≥80%) adherence groups, with statistical significance set at p<0.05.
Results
Compared to the good adherence group, patients with poor adherence were more likely to be aged 50 or older, to have received aromatase inhibitors (AIs) monotherapy, and to have not undergone radiation therapy. No significant differences were observed between the two groups in terms of sex or family history of breast cancer (Table 1 [Tab. 1]).
Table 1: Patient demographics and clinical characteristics in breast cancer cases from Asan Medical Center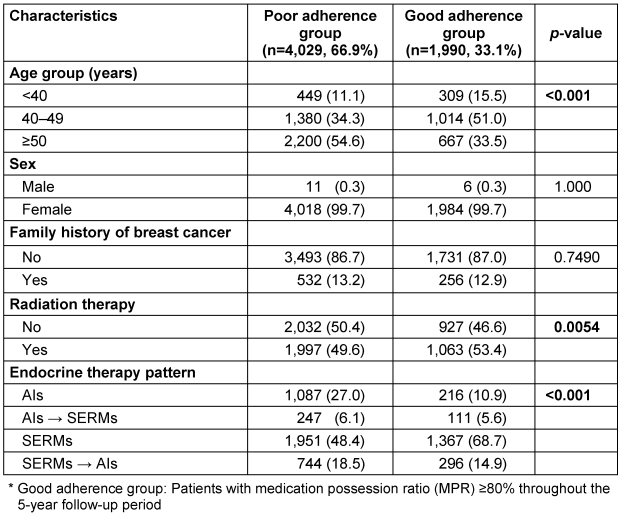
Over the five-year follow-up period, the proportion of patients with poor adherence increased from 3.9% in year 1 to 54.2% in year 5. Notably, sharp declines in adherence were observed between years 1 and 2, and again between years 4 and 5. In year 5, adherence was highest among patients aged 40–44, while lower rates were observed in those over 70 and in younger patients aged 20–24. Among the four endocrine therapy patterns, patients who switched from SERMs to AIs maintained the highest adherence, whereas those on AIs monotherapy had the lowest, declining to approximately 56% by year 5 (Figure 1 [Fig. 1]).
Figure 1: Five-year trends in medication possession ratio (MPR) by age group and endocrine therapy pattern among breast cancer patients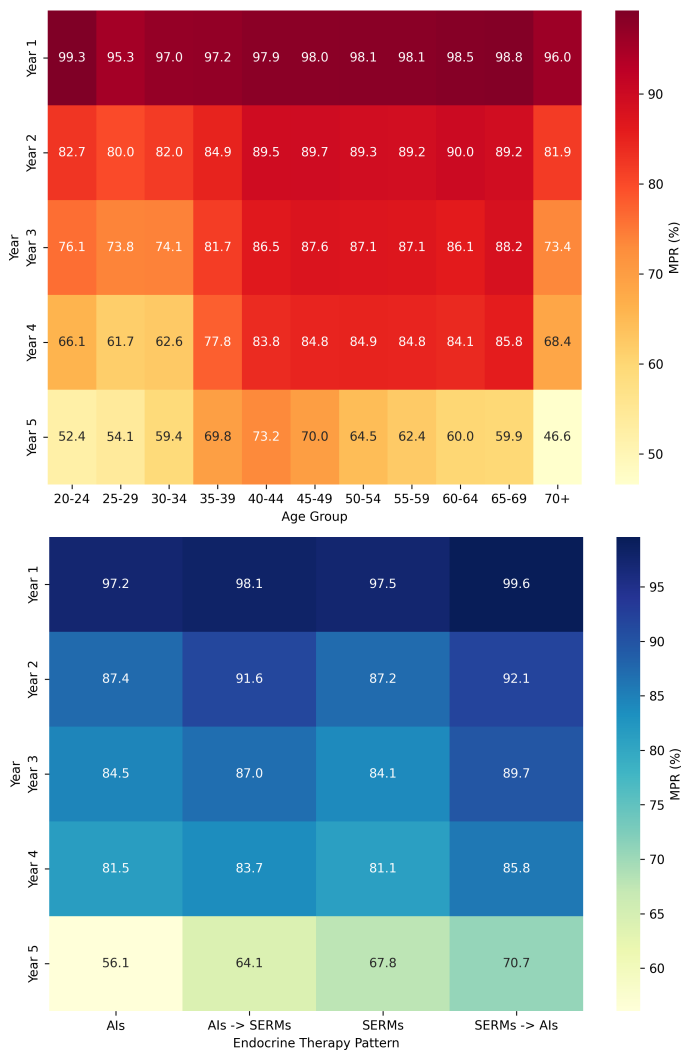
Discussion
Medication adherence steadily declined from 97% to 66% over five years, with sharp drops observed between years 1–2 and 4–5. These trends highlight the need for sustained support throughout long-term therapy. Adherence varied by age and treatment type: older patients (≥70) showed lower rates, while those who switched from SERMs to AIs had the highest. In older patients, reduced adherence may result from adverse effects related to polypharmacy, whereas in younger patients, pregnancy and childbirth may contribute to nonadherence.
A limitation of this study is the inability to distinguish between medically intended discontinuation (e.g., due to adverse effects or physician judgment) and true nonadherence, as such details were not available in the EHR dataset. However, the use of breast cancer-specific registry data curated by clinical experts in future research may enable more accurate identification of these cases. Despite this limitation, our study provides valuable real-world evidence on long-term AET adherence in a large breast cancer cohort.
In future research, we plan to apply machine learning models to identify predictive factors of adherence and stratify patient risk. These findings will inform the development of AI-driven digital tools – such as personalized adherence reminders, risk alerts, and intelligent monitoring systems – to support long-term medication adherence in clinical practice.
Notes
Authors’ ORCIDs
- Suyeon Kim: 0009-0003-7979-9280
- Ye-Eun Park: 0000-0003-1190-7882
- Yura Lee: 0000-0003-2048-3727
- Jong Won Lee: 0000-0001-7875-1603
Competing interests
The authors declare that they have no competing interests.
References
[1] Camejo N, Castillo C, Tambasco C, Strazzarino N, Requena N, Peraza S, Boronat A, Herrera G, Esperon P, Cuello M, Krygier G. Assessing Adherence to Adjuvant Hormone Therapy in Breast Cancer Patients in Routine Clinical Practice. World J Oncol. 2023 Aug;14(4):300-8. DOI: 10.14740/wjon1647[2] McCowan C, Wang S, Thompson AM, Makubate B, Petrie DJ. The value of high adherence to tamoxifen in women with breast cancer: a community-based cohort study. Br J Cancer. 2013 Sep 3;109(5):1172-80. DOI: 10.1038/bjc.2013.464
[3] Eliassen FM, Blåfjelldal V, Helland T, Hjorth CF, Hølland K, Lode L, Bertelsen BE, Janssen EAM, Mellgren G, Kvaløy JT, Søiland H, Lende TH. Importance of endocrine treatment adherence and persistence in breast cancer survivorship: a systematic review. BMC Cancer. 2023 Jul 4;23(1):625. DOI: 10.1186/s12885-023-11122-8
[4] Kaur N, Gonzales Iv M, Alcaraz CG, Gong J, Wells KJ, Barnes LE. A computational framework for longitudinal medication adherence prediction in breast cancer survivors: A social cognitive theory based approach. PLOS Digit Health. 2025 Jun 10;4(6):e0000839. DOI: 10.1371/journal.pdig.0000839
[5] Liao WC, Angus F, Conley J, Chen LC. The Efficacy of Digital Interventions on Adherence to Oral Systemic Anticancer Therapy Among Patients With Cancer: Systematic Review and Meta-Analysis. JMIR Cancer. 2025 Apr 16;11:e64208. DOI: 10.2196/64208




